US Pharm.
2008;33(1):27-31.
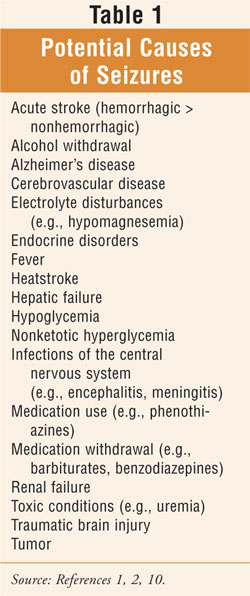
A variety of neurologic
conditions present more often in individuals of advancing age. Among seniors,
the majority of seizure disorders are secondary to symptomatic causes
(TABLE 1) that are frequently age-related. In some instances, if an
underlying etiology is identified and corrected, the patient may not require
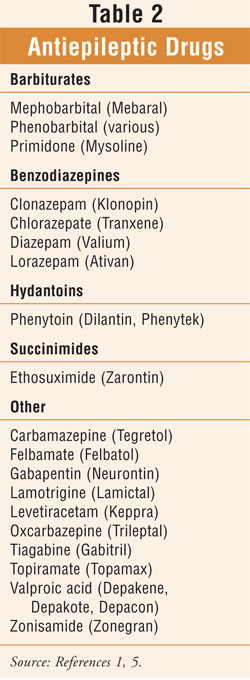
long-term antiepileptic drug (ED) therapy (TABLE 2).1 In
light of the high incidence of polypharmacy among the elderly, drug-induced
seizures may be a particular risk for this population. There is a relatively
high frequency of epilepsy in the elderly that is now being recognized.1
While new-onset seizures are uncommon in geriatric patients, according to one
study the three most common identifiable causes of acute symptomatic seizures
in adults were alcohol withdrawal, strokes, and electrolyte disturbances.2
Among all age groups, the most clearly established risk factors for epilepsy
are central nervous system (CNS) infections, stroke, and head trauma.1
Specifically in the elderly, cerebrovascular disease is the most common cause
of seizure activity, with 10% of patients having epileptic seizures poststroke.
2 The principle strategy in treating epileptic seizures, if possible, is
to treat the underlying cause.2 Pharmacists should become familiar
with the therapeutic goal of therapy and the potentially avoidable and
treatable causes of seizures in the elderly.
Seizure Disorders
Seizures and
epilepsies are often referred to by the umbrella term seizure disorders.
The term seizure is nonspecific and is the label for a sudden
transient change in the function of the brain caused by a variety of
conditions.2 Epilepsy is the label used for any CNS disorder
that causes a predisposition to recurrent seizures.2 A
persistent chronic abnormality is implicated with a diagnosis of epilepsy.
Symptoms of a seizure are dependent upon the seizure type. Even though
seizures can vary from individual to individual, they tend to be stereotyped
within a patient. Generalized tonic-clonic seizures (GTCs), classified as
major convulsive episodes, are always accompanied by a loss of
consciousness. Complex partial seizures may produce somatosensory or focal
motor features and are associated with altered consciousness. Finally, absence
seizures can typically appear bland, with extremely brief (i.e., seconds)
periods of altered consciousness.1 Between seizure episodes, there
are usually no objective signs of epilepsy.1
Cerebrovascular Disease and
Dementia
The most common cause of seizure
activity in seniors is cerebrovascular disease, occurring more frequently as a
consequence of a hemorrhagic stroke than the nonhemorrhagic type.2
ÜMost early seizures (i.e., <2 weeks) manifest within the first 24 to 48 hours
of a stroke, and only a small percentage of patients develops epilepsy.2
ÜIt has been suggested that late-onset epilepsy may be related to clinically
silent strokes.
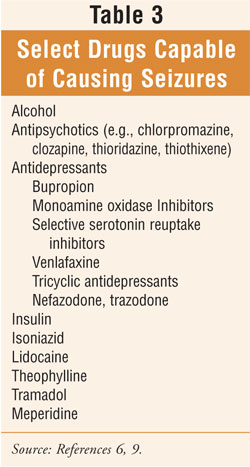
Drug-Induced Seizures
A variety of drugs have been
associated with the onset of seizures (TABLE 2) In a hospital-based
study, isoniazid and psychotropic medications were the most frequent
provocative cause of drug-induced seizures; bronchodilators, insulin,
isoniazid, and lidocaine tended to cause multiple seizures.2 The
researchers reported GTC seizures in 96% of all patients, while a minority of
the seizures were partial with secondary generalization.2
Antipsychotics
All patients receiving antipsychotic
therapy are at increased risk for drug-induced seizures. The risk is increased
further if the patient has: 1) a pre-existing seizure disorder; 2) a history
of drug-induced seizures; 3) an abnormal electroencephalogram (EEG); and 4) a
pre-existing pathology of the CNS or head trauma.3 Seizures
associated with antipsychotic agents are more likely to arise upon initiation
of therapy and when higher doses or rapid titration are utilized.3
Clozapine and chlorpromazine carry the highest risk potential of all the
antipsychotics according to reports, and olanzapine may also be associated
with greater risk based on EEG findings.3 If an isolated
antipsychotic-induced seizure occurs, anticonvulsant therapy is not
recommended; rather, a reduced antipsychotic dosage is advised.3 If
a change in antipsychotic is warranted, agents with the lowest potential to
lower seizure threshold are recommended (e.g., risperidone, haloperidol,
fluphenazine, pimozide, molindone, trifluoperazine, thioridazine).4
Antidepressants
Antidepressant drugs (TABLE 3
) vary in their potential to cause risk of seizures associated with therapy.
5,6 In particular, bupropion can cause seizures in 0.4% of patients
taking daily doses of 450 mg or less.6-8 Bupropion is
contraindicated in patients with a history of seizure disorder.5,6
The tetracyclic antidepressant maprotiline is associated with a higher
incidence of seizures compared with standard tricyclic antidepressants.
Traumatic Brain Injury
Seizures may occur
as a neurological consequence of traumatic brain injury (TBI). In a small
percentage of TBI patients, late seizures may develop (>7 days after injury)
weeks, months, or even years after the insult.9 Most seizures start
within the first one to two years following injury.2 Since
prolonged seizure activity may result in increased intracranial pressure and
worsen brain damage, it should be prevented, if at all possible, and promptly
treated.9 In patients with significant structural damage (e.g.,
brain lacerations, hematomas), a prophylactic anticonvulsant should be
considered (e.g., phenytoin).9 Treatment duration varies, depending
on the type of injury and results of the EEG. In general, anticonvulsants
should be discontinued within one week if no seizures have developed because
the value of anticonvulsant therapy in preventing future seizures is not
established; current studies are evaluating newer agents.9
Heatstroke
Hyperthermia,
accompanied by a systemic inflammatory response causing multiple organ
dysfunction and often death, is referred to as heatstroke. Injectable
benzodiazepines (e.g., lorazepam or diazepam) may be used to prevent seizures,
which may occur during the cooling phase of treatment for this condition.
9
Hypomagnesemia
Hypomagnesemia is defined as a low
plasma magnesium (Mg) level (<1.4 mEq/L [<0.70 mmol/L]) secondary to
inadequate Mg intake and absorption, or increased excretion due to
hypercalcemia or medications such as furosemide.9 Severe
hypomagnesemia (Mg < 1 mEq/L [<0.5 mmol/L]) produces generalized seizures
requiring aggressive magnesium replacement.
Miscellaneous Issues
Dental care for the seizure patient
should include the use of chlorhexidine topical rinses (e.g., Peridex,
generic) in those who are unable to brush or floss effectively.9
When dental appliances are required, the nonremovable type is recommended to
avoid swallowing or aspirating them.9
Treatment
There is clinical
controversy regarding the most appropriate time to initiate AED therapy.1
There are clinicians who initiate treatment only after a second unprovoked
seizure has arisen. Some clinicians initiate AED therapy after the onset of a
first seizure and others utilize treatment prophylactically in patients who
have experienced insult to the CNS that will probably evolve into epilepsy,
such as a stroke or TBI.1 Specific circumstances and individual
patient characteristics usually drive the decisions surrounding appropriate
AED treatment on a case-by-case basis.
Ultimately, the treatment goal
for epilepsy is no seizures and the absence of side effects with an optimal
quality of life.1 When AEDs are used to treat epilepsy in seniors,
age-related pharmacokinetic (PK) and pharmacodynamic (PD) changes must be
considered. Concurrent medications in the geriatric medication regimen may
reduce absorption of certain AEDs, thereby decreasing their bioavailability.
2 Due to an elderly individual's lower concentration of circulating
plasma proteins (i.e., albumin), an increase in the free fraction of
circulating AEDs with high protein-binding affinities is likely. Because of
this, it is usually more beneficial to measure free AED levels rather
than routine total AED levels in the elderly.2 There is also
a potential for increased AED concentration for a given dose due to a reduced
volume of distribution secondary to lower amounts of total body water in older
individuals. The volume of distribution for fat-soluble drugs is greater in
seniors due to an increased ratio of fat to lean muscle, which may ultimately
prolong the elimination half-life of AEDs. Elevated serum half-lives are
likely with AEDs that are extensively metabolized by the liver (e.g.,
carbamazepine, phenytoin, phenobarbital, sodium valproate) due to a reduction
in clearance in seniors (i.e., secondary to age-related decreased hepatic
mass, blood flow, and cytochrome P-450 activity). Decreased renal clearance in
the elderly (i.e., secondary to age-related decreased renal mass, blood flow,
and glomerular filtration) may cause problems with newer generation AEDs that
are primarily renally excreted (e.g., gabapentin, topiramate). Seniors are
typically pharmacodynamically more sensitive to the therapeutic and toxic
effects of AEDs.2 In addition to the above-mentioned PK and PD
issues, comorbidities and polypharmacy associated with geriatric
pharmacotherapy should be considered when an AED is implemented; initial doses
should be conservative and titration should be slow. Although it is beyond the
scope of this article to discuss the pharmacologic management of epilepsy in
detail, the reader is referred to Reference 1 for a comprehensive presentation
of the topic.
Conclusion
With the advancement of age, several
neurologic disorders present more frequently, and seniors are especially
susceptible to seizures and epilepsy. The high incidence of cerebrovascular
disease and polypharmacy in seniors places them at particular risk.
Pharmacists should be familiar with the symptomatic treatable causes of
seizures, including those that are drug-induced, particularly since
polypharmacy is a significant concern among geriatric patients. With the
advancement of age, several neurologic disorders present more frequently, and
seniors are especially susceptible to seizures and epilepsy. The high
incidence of cerebrovascular disease and polypharmacy in seniors places them
at particular risk. Pharmacists should be familiar with the symptomatic
treatable causes of seizures, including those that are drug-induced,
particularly since polypharmacy is a significant concern among geriatric
patients.
References
1. Gidal BE, Garnett Wr. Epilepsy. In: DiPiro JT, Talbert RL, Yee GC, et al., eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York, NY: McGraw-Hill; 2005:1023-1048.
2. Ferrendelli AJ, Lim HL. Epilepsy in the elderly. In: Hazzard WR, Blass JP, Halter JB, et al., eds. Principles of Geriatric Medicine and Gerontology. 5th ed. New York, NY: McGraw-Hill, Inc.; 2003:1431-1441.
3. Crismon ML, Buckley PF. Schizophrenia. In: DiPiro JT, Talbert RL, Yee GC, et al., eds. Pharmacotherapy: A Pathophysiologic Approach, 6th ed. New York: McGraw-Hill; 2005:1225.
4. Pisani F, Oteri G, Costa C, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25:91-110.
5. Semla TP, Beizer JL, Higbee MD. Geriatric Dosage Handbook. 12th ed. Hudson, OH: Lexi-Comp, Inc.; 2007.
6. Kando JC, Wells BG, Hayes PE. Depressive disorders. In: DiPiro JT, Talbert RL, Yee GC, et al., eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York, NY: McGraw-Hill; 2005:1241.
7. Johnston JA, Lineberry CG, Ascher JA. A 102 center prospective study of seizures in association with bupropion. J Clin Psychiatry. 1991;52:450-456.
8. Nierenberg AA, Cole JO. Antidepressant adverse drug reactions. J Clin Psychiatry. 1991;52(suppl):40-47.
9. Beers MH, Porter RS, Jones TV, et
al. The Merck Manual of Diagnosis and Therapy. 18th ed. Whitehouse
Station, NJ: Merck Research Laboratories; 2006:849,1262-1263,
1709,2543,2609.
10. Beers MH, Berkow R, eds.The
Merck Manual of Geriatrics. 3rd ed. Whitehouse Station, NJ: Merck & Co.;
2000:176,235,359,380-381.





