US Pharm. 2007;32(9):54-56.
The
periodontium, defined as the tissues that surround and support the teeth,
includes the gingivae (gums), bone, cementum (root surface), and periodontal
ligament (fibers that hold the tooth in the socket). Many oral health changes
to the periodontium occur during the lifetime of a female, starting at puberty
and progressing through menstruation, pregnancy, and menopause. These changes
are due to alterations in the level of sex hormones, such as progesterone and
estrogen.
Sex Hormones and
Periodontal Changes
Estrogen, which is
secreted by the ovaries, is important for the development and maintenance of
secondary sex characteristics and for uterine growth. Progesterone, which is
secreted by the corpus luteum and the placenta, is responsible for building
the uterine lining in the second half of the menstrual cycle and during
pregnancy. Both hormones have an effect on periodontal tissues and periodontal
disease progression (e.g., gingivitis and periodontitis).1,2
Receptors for estrogen and
progesterone are pres ent in the gingiva.2,3 Elevated levels
of progesterone are responsible for increased vascular dilation of the
gingival tissues, the production of prostaglandins, and the movement of
polymorphonuclear leukocytes, all of which result in gingival inflammation.
Estradiol increases the amount of gingival inflammation with no increase of
bacterial plaque.2 Many periodontal bacteria residing in the
subgingival environment, such as black-pigmented Bacteroides,
Prevotella intermedia, and the Capnocytophaga species, utilize
estradiol (principal estrogen) and progesterone as growth factors or
nutrients. Additionally, in a study by Contreras et al., a higher proportion
of preeclamptic women were infected in the gingival pockets with periodontal
pathogens such as Porphyromonas gingivalis, Tannerella forsythensis
, and Eikenella corrodens, compared with nonpreeclamptic or normal
pregnant women.4
Hormonal fluctuations during a
female's lifetime may cause an exaggerated inflammatory response to dental
plaque, resulting in gingivitis. Features of hormone-associated gingivitis
include accumulation of dental plaque on the teeth, pronounced inflammation of
the gingivae, redness of the gingivae, and bleeding gingivae. These changes
vary depending on the individual and are most likely related to the
individual's immune response to various irritants (e.g., dental plaque) in the
mouth. Thus, a female with elevated hormone levels and minimal bacterial
plaque in the mouth may have an exaggerated response to the plaque irritant
and thereby develop gingivitis. Hormone associated-gingivitis is reversible
following puberty or pregnancy, and no radiographic bone loss is observed.
Approximately 23% of women
between the ages of 30 and 54 have periodontitis, which is characterized by
pocket formation and bone loss around the teeth. About 44% of women between
the ages of 55 and 90 with periodontitis still have their teeth.5
As a woman's health changes throughout her lifetime, oral health can change as
well. Pubertal girls, women of childbearing age, and pregnant women have
elevated levels of progesterone, primarily, but also of estrogen. These
elevated hormone levels have certain oral health implications. In addition,
menopausal and postmenopausal women have decreased sex hormone levels, which
also have certain oral health implications.
Puberty
During puberty,
increased levels of progesterone and, possibly, estrogen may have effects on
the gingivae. Puberty-associated gingivitis is characterized by swollen, red,
bleeding gingivae.6 These soft tissue changes are transitory and
revert to normal levels in the post-circumpubertal period. Most females with
healthy gingivae likely will not develop significant periodontal changes.
A higher population of
bacteria in subgingival pockets is present during puberty, which may
selectively accumulate estradiol and progesterone.2 Meticulous oral
home care consisting of regular brushing and flossing and routine dental
visits may help prevent the development of gingivitis.
Menstruation
During the luteal
phase of the menstrual cycle, which begins at about day 14 of the cycle and
then declines, progesterone levels peak. Elevated levels of progesterone may
cause significant oral inflammatory changes, such as bleeding and red, swollen
gingivae. Thus, gingival changes may occur just before the beginning of the
period and disappear once it begins.7 Most females with healthy
gingivae likely will not develop significant periodontal changes. Changes in
estradiol levels during the menstrual cycle may also be accompanied by similar
fluctuations in bacterial flora.
Pregnancy
Pregnancy-associated gingivitis can occur in approximately 57% of pregnant
women.8 During pregnancy, there is a marked elevation in sex
hormones, which may affect the gingival tissues in certain individuals. An
exaggerated gingival inflammatory response to dental plaque is the primary
cause of the gingivitis, which usually starts around the second month of
pregnancy and generally resolves following parturition (Figure 1).
Additionally, pregnancy may accelerate the development of periodontitis (deep
pockets and bone loss around teeth).9 There may also be a link
between periodontitis and adverse pregnancy outcomes, including preterm
delivery and low-birth-weight babies.10
Periodontal treatment of the
pregnant patient has been controversial. Findings from one clinical study
reported that periodontal treatment during the second and third trimesters of
pregnancy is safe, but the risk of adverse effects, such as preterm delivery
(birth occurring before 37 weeks of pregnancy), low birth weight, fetal growth
restriction, or preeclampsia, is not reduced.11,12 On the other
hand, data from four clinical trials found that periodontal treatment in
pregnant women may lower the incidence of preterm delivery and
low-birth-weight babies.13 Maternal and fetal exposures to
gram-negative periodontal bacteria may trigger inflammatory events in both the
mother and the fetus, which may stimulate early rupture of membranes and
parturition.13
Oral Contraceptives
Oral contraceptives
act by elevating hormone levels, simulating pregnancy to prevent ovulation.
Thus, it is expected that the same gingival changes seen during pregnancy will
also be seen in women taking oral contraceptives. Newer oral contraceptive
formulations contain a lower concentration of hormones, resulting in a milder
inflammatory response of the gingivae to dental plaque.14
Menopause
Menopause by itself
is not a risk factor for periodontal diseases. A correlation between
osteoporosis and periodontal disease and tooth loss in postmenopausal women
has been documented but is not considered a definitive risk factor.15
Skeletal bone mineral density is related to loss of bone around the teeth.
16 Since the teeth are embedded in bone that comprises the maxilla and
mandible, osteoporotic changes may affect these structures.
The use of intravenous and
oral bisphosphonates has been linked to an increased incidence of
osteonecrosis of the jaws in patients undergoing dental procedures such as
tooth extractions, periodontal surgery or cleanings, and root canals.17-19
Bisphosphonate-associated osteonecrosis of the jaws is characterized by pain
or swelling in the affected jaw, an irregular mucosal ulceration with exposed
bone in the mandible or maxilla, and infection. It is important for the
pharmacist and dentist to be aware that the patient will be or currently is
taking a bisphosphonate. Commonly prescribed bisphosphonates include
zolendronic acid (Zometa), pamidronate (Aredia), alendronate (Fosamax),
ibandronate (Boniva), risedronate (Actonel), tiludronate (Skelid), clodronate
(Bonefos), and etidronate (Didronel).
Additional oral symptoms
experienced by postmenopausal women include burning oral sensations--especially
on the tongue--altered taste sensations, and a decrease in salivary flow. If
xerostomia is present, dental plaque may accumulate secondary to reduced
salivary function/flow, leading to caries and, possibly, gingivitis. Salivary
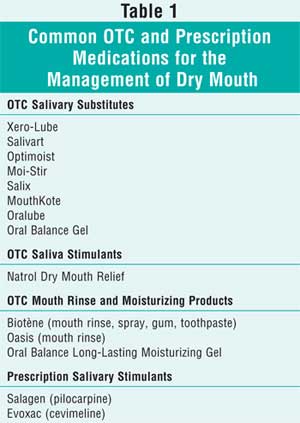
substitutes that help reduce oral dryness are listed in Table 1.
Coronary Heart Disease
During the late
1990s, a correlation was found between periodontitis and cardiovascular
disease,20 which some researchers attributed to lifestyle changes.
Others claim there is a systemic inflammatory response that causes an invasion
of periodontal bacteria into the muscle cells in the arteries, resulting in
platelet aggregation.21,22 A study in 2005 reported that women with
coronary heart disease have worse oral health than those with no history of
coronary heart disease.22 The authors concluded that although the
reason is unclear, the inflammation in the periodontium may trigger and
influence the atherosclerotic process.22,23 More research is needed
to further justify these findings.
Summary
Sex hormones are
associated with the onset and progression of periodontal disease. As levels of
estrogen and progesterone elevate during puberty, menstruation, and pregnancy,
so does the prevalence of gingivitis. Pharmacists with patients who are
pregnant or planning to become pregnant should be counseled on proper oral
home care and the importance of regular visits to a dentist or periodontist
for a comprehensive periodontal exam. Also, it is important to try to identify
periodontal risk factors and to offer treatment to help reduce the rate of
premature births. Reduction of the inflammatory component may help decrease
the risk of adverse pregnancies.24
New York is the first state to
have guidelines for the oral health care of women of childbearing years.
Specific advisory statements have been published assisting prenatal care
providers and oral health professionals in the welfare of pregnant women.
25
Pharmacists should counsel
patients who take or will be taking bisphosphonates on the importance of
receiving a dental examination prior to initiating bisphosphonate therapy.
Patients should complete any nonelective dental procedures prior to starting
therapy and have routine dental visits during bisphosphonate therapy.
References
1. Mascarenhas P, Gapski R, Al-Shammari K, Wang HL. Influence of sex hormones on the periodontium. J Clin Periodontol. 2003;30:671-681.
2. Güncü GN, Tözüm TF, Caglayan F. Effects of endogenous sex hormones on the periodontium--review of literature. Aust Dent J. 2005;50:138-145.
3. Sooriyamoorthy M, Gower DB. Hormonal influences on gingival tissue: relationship to periodontal disease. J Clin Periodontol. 1989;16:201-208.
4. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontal. 2006;77:182-188.
5. Albandar JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. J Periodontol. 1999;70:13-29.
6. Califano JV; Research, Science and Therapy Committee American Academy of Periodontology. Position paper: periodontal diseases of children and adolescents. J Periodontol. 2003;74:1696-1704.
7. Machtei EE, Mahler D, Sanduri H, Peled M. The effect of menstrual cycle on periodontal health. J Periodontol . 2004;75:408-412.
8. Leiff S, Boggess KA, Murtha AP, et al. The oral conditions and pregnancy study: periodontal status of a cohort of pregnant women. J Periodontol. 2004;75:116-126.
9. Moorse S, Randhawa M, Ide M. A case-control study to investigate an association between adverse pregnancy outcome and periodontal disease. J Clin Periodontol. 2005;32:1-5.
10. Jeffcoat MK, Hauth JC, Geurs NC, et al. Periodontal disease and preterm birth: results of a pilot intervention study. J Periodontol. 2003;74:1214-1218.
11. Michalowicz BS, Hodges JS, DiAngelis AJ, et al. Treatment of periodontal disease and the risk of preterm birth. New Engl J Med. 2006;355:1885-1894.
12. Scannapieco FA, Bush RB, Paju S. Periodontal disease as a risk factor for adverse pregnancy outcomes. A systematic review. Ann Periodontol. 2003;8:70-78.
13. Paquette DW. Periodontal disease and the risk for adverse pregnancy outcomes. Grand Rounds Oral-Sys Med. 2006;4:14-25.
14. Preshaw PM, Knutsen MA, Mariotti A. Experimental gingivitis in women using oral contraceptives. J Dent Res . 2001;80:2011-2015.
15. Oh TJ, Bashutski J, Giannobile W. The interrelationsip between osteoporosis and oral bone loss. Grand Rounds Oral-Sys Med. 2007;2:10-21.
16. Tezal M, Wactawski-Wende J, Grossi SG, et al. The relationship between bone mineral density and periodontitis in postmenopausal women. J Periodontol. 2000;71:1492-1498.
17. American Association of Endodontists. Bisphosphonate-associated osteo necrosis of the jaw. Winter 2007. Available at: www.aae.org/NR/rdonlyres/9E3AB124-D83B-41DA-B8D2-260B3971802E/0/winter07ecfe.pdf.
18. American Association of Oral and Maxillofacial Surgeons. Position paper on bisphosphonate-related osteonecorsis of the jaws. September 25, 2006.
19. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff S. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527-534.
20. Beck JD, Offenbacher S. Oral health and systemic disease: periodontitis and cardiovascular disease. J Dent Educ. 1998;62:859-870.
21. Shanies S, Hein C. The significance of periodontal infection in cardiology. Grand Rounds Oral-Sys Med. 2006;1:24-33.
22. Buhlin K, Gustafsson A, Ahnve S, et al. Oral health in women with coronary heart disease. J Periodontol. 2005;76:544-550.
23. Dorn BR, Dunn WA, Progulski-Fox A. Invasion of human coronary artery cells by periodontal pathogens. Infect Immun. 1999;67:5792-5798.
24. Kerpen SJ, Fleischer A. An obstetrician and periodontist translate periodontal systemic research to preserve the health of pregnant women at risk for adverse pregnancy outcomes. Grand Rounds Oral-Sys Med. 2006;4:18-38.
25. Burakoff R. New York State
leading the way in establishing guidelines for oral care in pregnancy.
Grand Rounds Oral-Sys Med. 2006;4:50-52.
To comment on this article, contact
editor@uspharmacist.com.





