US Pharm. 2006;11:31-38.
Posttraumatic stress disorder (PTSD)
is a severe and chronic condition, with a lifetime prevalence of 1.3% to 7.8%
in the general population.1 The three main characteristics and
diagnostic criteria for PTSD are symptoms of reexperiencing, numbing and
avoidance, and hyperarousal.2 PTSD occurs after an individual
experiences, witnesses, or is confronted with a traumatic event. Common
examples of traumatic events that can lead to PTSD are war combat, motor
vehicle accidents, sexual abuse, violent crimes, terrorist attacks, natural
disasters, and a sudden or unexpected loss of a loved one.
Diagnosis and Symptoms
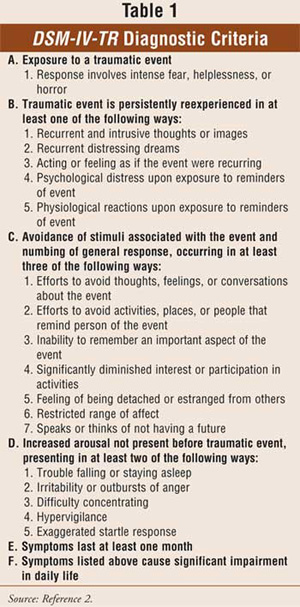
The Diagnostic
and Statistical Manual of Mental Disorders (DSM-IV-TR) classifies
PTSD as an anxiety disorder. The full diagnostic criteria can be found in
Table 1. If symptoms last less than three months, the condition is
diagnosed as acute PTSD. If symptoms last more than three months, it is
considered chronic PTSD.2 About 33% to 50% of PTSD cases
will become chronic. The usual onset of symptoms is within six months of the
traumatic event; otherwise, it is categorized as PTSD with delayed onset
.
Reexperiencing can take on
different forms. The patient can have recurrent and intrusive thoughts about
the event, suffer nightmares relating to the experience, and act or feel as if
the traumatic event was reoccurring. These patients also have psychological
and physiological responses to reminders of the traumatic event, such as an
anniversary of the event, a news story where a similar event has occurred, or
a location similar to where the traumatic event took place. It is not uncommon
for war veterans to become psychologically and physiologically distressed when
they witness news about ongoing wars.
Persistent symptoms of
increased anxiety or hyperarousal are also diagnostic criteria for PTSD. These
symptoms can include difficulty with sleep, irritability, outbursts of anger,
difficulty concentrating, hypervigilance, and an exaggerated startled
response. Patients tend to state that they are always "jumpy" or "on edge."
Patients with PTSD also avoid
any reminders of the trauma and appear numb in their mood, making great
efforts to avoid thoughts, feelings, conversations, activities, places, or
people that they associate with the traumatic event. They may have an
inability to recall important parts of the trauma. People with PTSD may become
isolated and detached from others, lose interest in activities they used to
enjoy, or have a restricted affect.
Symptoms of PTSD due to combat
have been described as far back as the American Civil War.3 PTSD
became more prevalent after the Vietnam War, with 15% of men and 31% of women
who were in combat developing it.4 In more recent wars, such as the
Gulf War, there is an estimated prevalence of 5.4% to 12.1%.5
Motor vehicle accidents and
sexual abuse are two causes of PTSD that are seen commonly by primary care
physicians. It is estimated that 9% people involved in a motor vehicle
accident will develop PTSD, making it one of the leading causes of PTSD in the
United States.1
Unfortunately, PTSD often goes
unrecognized in the primary care setting. One study reviewed 2,975 Israeli
patients and found that only 2% of those who met the criteria for PTSD were
actually diagnosed with it.6 A better understanding of the causes
and symptoms of PTSD would allow these patients to be diagnosed earlier and
therefore receive treatment earlier.
One of the problems of
treating PTSD is that a large percentage of these patients also have a second
psychiatric diagnosis. It is estimated that 79% of women and 88% of men have
at least one other psychiatric diagnosis, and 49% of women and 59% of men have
at least three psychiatric diagnoses. Among Vietnam War veterans, 98.9% have a
second psychiatric diagnosis. These patients also have a higher risk of other
mental illnesses, such as social phobia and panic attacks. Alcohol and drug
abuse are also common in these patients; 52% of men and 28% of women suffer
from alcohol abuse, and 35% of men and 27% of women suffer from concurrent
drug abuse.7
Treatment for PTSD
Treatment of PTSD
consists of pharmacotherapy to treat symptoms, as well as psychotherapy
interventions, such as cognitive behavioral therapy (CBT). A combination of
both pharmacologic and psychological treatment is the preferred approach. The
goal of treatment is to reduce the frequency and severity of symptoms, improve
social functioning, and relieve comorbid psychiatric disorders associated with
PTSD, such as depression, anxiety, panic attacks, and bipolar disorder.8
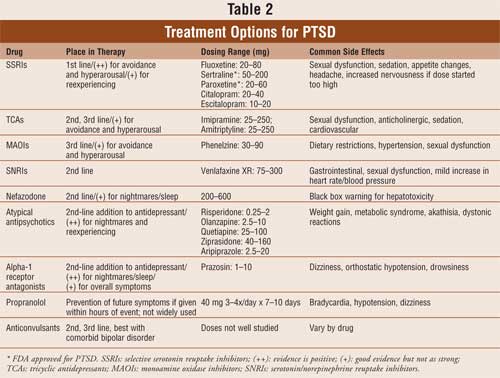
Antidepressants:
Selective serotonin reuptake inhibitors (SSRIs) are considered first-line
therapy for PTSD, due to treatment guideline recommendations9 and
numerous double-blind placebo-controlled trials. Paroxetine and sertraline are
the only two antidepressants with an FDA-approved indication for the treatment
of PTSD. However, any of the SSRIs are efficacious in its treatment. All other
agents discussed below are used off-label for treating the symptoms of PTSD.
In a pooled analysis of three
paroxetine placebo-controlled trials, paroxetine was significantly better than
placebo in response, remission rates, improvement in sleep disturbances, and a
reduction in all three symptom clusters of PTSD.10 Two large
placebo-controlled trials were conducted involving a total of 395 patients
with a diagnosis of PTSD who took sertraline. In both studies, there was a
statistically significant reduction in all three symptom clusters, as measured
by the Cli? nician Administered PTSD Scale. The rates of response in the two
trials were 53% and 60% for sertraline and 32% and 38% for placebo.11,12
In these two studies, women showed a better response to treatment than men,
although this has not been a consistent finding. In addition, Vietnam combat
veterans' symptoms tend to be more resistant to treatment. This may be due to
the severe and repetitive nature of their trauma. It has also been suggested
that veterans receiving a disability pension for PTSD may be reluctant to
report improvement, in fear that their benefits would be taken away.13
It may take four to six weeks
to see an initial response to treatment. Some cases may require a longer
period of time, such as six to nine months, before full benefits are seen from
SSRIs. In one study, patients enrolled in a double-blind, 12-week study who
were taking sertraline were continued on open-label treatment for 24 more
weeks. Fifty-eight percent of the patients categorized as nonresponders at the
end of the initial 12-week trial became responders by the end of the 24-week
open-label trial. P atients who responded to sertraline treatment in the
initial 12 weeks continued to improve with an additional 30% decrease in
symptoms.14
The serotonin/norepinephrine
reuptake inhibitor (SNRI) venlafaxine has also been shown to be beneficial in
the treatment of PTSD. Davidson et al. conducted a 12-week, double-blind trial
of 538 patients taking venlafaxine extended release (XR), sertraline, or
placebo.15 Venlafaxine XR did have a statistical significance over
placebo in reducing avoidance/numbing and hyperarousal. The improvement in
reexperiencing was not significantly better in either treatment group.
Remission rates were 30.2% with venlafaxine XR, 24.3% with sertraline, and
19.6% for placebo. However, in overall efficacy and tolerability, venlafaxine
XR and sertraline showed similar improvement. This is the only double-blind
study of venlafaxine in PTSD, but it shows promise for the SNRIs as a
treatment option in PTSD.
The tricyclic antidepressants
(TCAs) and monoamine oxidase inhibitors (MAOIs) have also been used for PTSD.
Amitriptyline was compared to placebo in 46 veterans over eight weeks, with
modest improvement in remission rates of 36% and 28%, respectively.16
Phenelzine and imipramine were shown to be equally efficacious in overall
symptom improvement in a randomized double-blind trial, with 64% and 75% of
patients on phenelzine and imipramine showing improvement, respectively.17
Another trial comparing phenelzine, imipramine, and placebo demonstrated a
response of 44%, 25%, and 5%, respectively.18 Although both of
these drug classes appear to be effective, they are not often used due to
their high incidence of side effects and patients' inability to tolerate them.
In particular, MAOIs have dietary restrictions and are linked to the risk of
hypertensive crisis, while TCAs have anticholinergic and cardiovascular side
effects. In a retrospective analysis of veterans with PTSD and major
depression, Dow and Kline19 showed that the majority of respondents
were treated with SSRIs (23 of 32 patients). Imipramine was the most
successful TCA in this analysis (four of 32 patients). Currently, these TCAs
and MAOIs are considered as second- or third-line agents restricted for
treatment-resistant cases.
Nefazodone has been compared
to sertraline in a double-blind trial and shown to be comparable.20
Because of its mechanism of action, nefazodone may have a beneficial effect on
sleep-related symptoms of PTSD, such as nightmares.21 However,
nefazodone carries a black box warning for hepatotoxicity; therefore, caution
should be used when prescribing this agent.
Other antidepressants, such as
trazodone, bupropion, and mirtazapine, have limited and inconclusive data in
association with PTSD. Their use is currently not recommended.
Overall, SSRIs are considered
first-line agents when treating patients with PTSD. Hyperarousal and
numbing/avoidance are the PTSD symptoms that respond best to treatment with
SSRIs, while reduction in nightmares and reexperiencing symptoms tend to be
less treatable. Common side effects with SSRIs include nausea, drowsiness,
insomnia, dry mouth, sexual dysfunction, and gastrointestinal distress. If a
patient does not respond to SSRI treatment, even after high doses, or cannot
tolerate SSRIs, other antidepressants such as venlafaxine, TCAs, or MAOIs can
be used. TCAs and MAOIs should not be considered as first-line agents due to
their side-effect profile.
Atypical Antipsychotics:
Atypical antipsychotics
have recently begun to be used in the treatment of PTSD. They appear to be
helpful in alleviating the reexperiencing cluster of symptoms. The atypical
antipsychotics are not FDA approved for the treatment of PTSD, but they do
appear to have a role in cases that are more severe, involve nightmares or
flashbacks that have not responded to other treatment, and/or when psychotic
symptoms may be present along with PTSD.
Risperidone, olanzapine,
quetiapine, ziprasidone, and aripiprazole are all linked to data showing
benefit in the treatment of PTSD, although none have an FDA indication for
such treatment.22-28 Monnelly et al.23 treated patients
with risperidone, and improvement was seen in nightmares, intrusive thoughts,
irritability, and total PTSD symptoms. Olanzapine and quetiapine have also
resulted in positive outcomes when used as adjunctive therapy to SSRIs.
25,26 A small amount of data suggests that the atypical antipsychotics
might even be beneficial as monotherapy in treatment-resistant patients with
psychotic features.29
From these studies, it appears
that adjunctive therapy with a low-dose atypical antipsychotic may be
effective in more resilient cases of PTSD, especially when the patient has
reexperiencing or psychotic symptoms that have had partial or no response to
treatment with SSRIs. If used, they are recommended as adjunctive therapy to
antidepressants. However, the patient should be informed of the possible side
effects associated with this class of medications, including hyperglycemia,
weight gain, increased appetite, lipid abnormalities, and extrapyramidal
symptoms. The association between atypical antipsychotics and metabolic
syndrome is well documented in the medical literature. The Consensus Statement
published by the American Diabetes Association contains information regarding
these risks and appropriate monitoring for patients.30
Benzodiazepines:
Benzodiazepines, although a common treatment in anxiety disorders, do not
seem to be beneficial in the treatment of PTSD symptoms. It would seem that
since benzodiazepines decrease arousal and promote sleep, they may be helpful
in PTSD, and although case reports and retrospective chart reviews seem to
support this role, double-blinded trials have failed to show their benefit.
31,32 In fact, an open-label trial found that not only are
benzodiazepines ineffective for PTSD, but they also may increase the risk of
PTSD and depression. Gelpin et al.33 attempted to use
benzodiazepines within 18 days of a traumatic event and followed patients for
six months. At the end of the study, nine of 13 benzodiazepine-treated
patients had developed PTSD versus three of 13 in the control group. In
addition, half of the patients in the benzodiazepine group developed
depression, compared to none in the control group.
Based on the evidence
available, it appears that benzodiazepines are not beneficial in the treatment
of PTSD. However, there are mixed results. If a patient has a comorbid illness
that may require benzodiazepines, such as panic attacks, then caution should
be used.
Adrenergic-Inhibiting
Agents: The
adrenergic-inhibiting agents are another option in the treatment of PTSD, used
best as adjunctive therapy. People with PTSD have been shown to have elevated
plasma levels of nor? epinephrine (NE).34 There is also
hyperactivity of NE in the brain when exposed to trauma-related stimuli.35
These two theories are the basis for the use of this class of medications. In
clinical trials, the alpha-1 receptor antagonist prazosin has been shown to
improve nightmares, sleep disturbances, and overall symptoms related to PTSD,
when given at night.36 New data suggest that daytime treatment with
prazosin may also alleviate symptoms of PTSD, particularly those related to
trauma cues.37
Beta-blockers, such as
propranolol, are also used in the treatment of PTSD. Unlike the other
medications discussed in this article, they are used to try to prevent
symptoms of PTSD. It is hypothesized that by blocking postsynaptic NE
receptors with beta-blockers, there will be a reduction in hormonally enhanced
memories and fear conditioning.35 Two trials showed decreased
physiologic response to reminders of trauma and fewer PTSD symptoms when
administered within six to 20 hours and maintained for 10 to 20 days.38,39
Although this practice is not done routinely, it could be a method of
preventing or lessening the symptoms of PTSD.
Anticonvulsants:
Anticonvulsants, or mood stabilizers, can be used for the treatment of bipolar
disorder. Although not used frequently in the treatment of PTSD, they may have
beneficial effects, particularly when patients have both PTSD and bipolar
disorder. Carbamazepine, valproic acid, topiramate, and gabapentin have all
been associated with positive data in open-label trials.40-43
Carbamazepine use helped
improve PTSD symptoms, including intrusive thoughts, flashbacks, and insomnia
in a combat veteran population, which is normally a tough population to treat.
40 Valproic acid improved hyperarousal and avoidance, but not intrusive
thoughts.41 Unfortunately, frequent monitoring and high incidence
of side effects limit the use of carbamazepine and valproic acid. However, if
a patient has comorbid PTSD and bipolar disorder, an anticonvulsant mood
stabilizer should be used. In one trial, topiramate helped reduce frequency of
nightmares in PTSD patients.42 Gabapentin, when used as adjunct
therapy, was found to reduce frequency of nightmares and insomnia.43
Gabapentin is generally well tolerated with mild side effects and thus might
be an effective option for adjunctive therapy. It is important to note that
none of these trials are double-blind placebo-controlled studies; therefore,
more rigorous trials are needed to better identify the role of anticonvulsants
in the treatment of PTSD. Lamotrigine is the only anticonvulsant tested in a
double-blind placebo-controlled trial.44 In a 12-week trial,
lamotrigine improved reexperiencing and avoidance/numbing. However, since this
trial had a small sample size, its results should be interpreted carefully.
Summary
Treatment options
for PTSD include antidepressants, atypical antipsychotics,
adrenergic-inhibiting agents, and anticonvulsants (see Table 2). The
target symptoms of pharmacologic therapy are hyperarousal, avoidance/numbing,
and reexperiencing. SSRIs are considered the first-line treatment option,
because these agents are generally well tolerated and have proven efficacy.
Sertraline and paroxetine are the only FDA-approved pharmacologic products for
the treatment of PTSD. Atypical antipsychotics can be used to reduce
reexperiencing and nightmares. They are best used as adjunctive therapy to
SSRIs. If patients cannot tolerate the first-line treatment options, other
antidepressants, such as venlafaxine, TCAs, and MAOIs, can be used. However,
TCAs and MAOIs are associated with numerous side effects. While terazosin, an
adrenergic-inhibiting agent, is helpful in reducing sleep-related disorders in
PTSD, the beta-blocker propranolol may be beneficial in preventing or reducing
PTSD symptoms if given shortly after the trauma. Benzodiazepines should
generally be avoided in this patient population unless it is necessary to
treat another comorbid disease. The treatment of PTSD is not simple. It may
require a long duration of pharmacologic treatment and should include
nonpharmacologic treatment, such as CBT or prolonged exposure therapy.
References
1. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psych. 1995;52:1048-1060.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Fourth edition. Text revision. Washington, DC: American Psychiatric Association; 2000. Ü
3. Dean E. Shook over Hell: Post-traumatic stress, Vietnam, and the Civil War. Cambridge, MA: Harvard University Press; 1997.
4. Kulka RA, Schlenger WE, Fairbank JA, et al. Trauma and the Vietnam War generation: report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel; 1990.
5. Kang HK, Natelson BH, Mahan CM, et al. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157:141-148.
6. Taubman-Ben-Ari O, Rabinowitz J, Feldman D, Vaturi R. Post-traumatic stress disorder in primary-care settings: prevalence and physicians' detection. Psychol Med. 2001;31:555-560.
7. Brady KT, Killeen TK, Brewerton T, et al. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61[Suppl 7]:22-32.
8. Davidson JRT. Pharmacological treatment of acute and chronic stress following trauma. J Clin Psychiatry . 2006;67[Suppl 2]:34-39.
9. Ballenger JC, Davidson JR, Lecruibier Y, et al. Consensus statement on posttraumatic stress disorder from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry. 2000;61[suppl 5]:60-66.
10. Stein DJ, Davidson J, Seedat S, Beebe K. Paroxetine in the treatment of post-traumatic stress disorder: pooled analysis of placebo-controlled studies. Expert Opin Pharmacother. 2003;4:1829-1838.
11. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283:1837-1844.
12. Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry. 2001;58:485-492.
13. Schoenfeld FB, Marmar CR, Neylan TC. Current concepts in pharmacotherapy of posttraumatic stress disorder. Psychiatric Serv. 2004;55:519-531.
14. Londborg PD, Hegel MT, Goldstein S, et al. Sertraline treatment of posttraumatic stress disorder: results of 24 weeks of open-label continuation treatments. J Clin Psychiatry. 2001;62:325-331.
15. Davidson J, Rothbaum BO, Tucker P, et al. Venlafaxine extended release in posttraumatic stress disorder: a sertraline- and placebo-controlled study. J Clin Psychopharmacol. 2006;26:259-267.
16. Frank JB, Kosten TR, Giller EL Jr, Dan E. A randomized clinical trial of phenelzine and imipramine for posttraumatic stress disorder. Am J Psychiatry. 1988;145:1289-1291.
17. Kosten T, Frank J, Dan E, et al. Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine. J Nerv Ment Dis. 1991;179:366-370.
18. Davidson K, Kudler H, Smith R, et al. Treatment of posttraumatic stress disorder with amitriptyline or placebo. Arch Gen Psychiatry. 1990;47:259-266.
19. Dow B, Kline N. Antidepressant treatment of posttraumatic stress disorder and major depression in veterans. Ann Clin Psychiatry. 1997;9:1-5.
20. McRae AL, Brady KT, Mellman TA et al. Comparison of nefazodone and sertraline for the treatment of posttraumatic stress disorder. Depress Anxiety. 2004;19:190-196.
21. Mellman TA, David D, Barza L. Nefazodone treatment and dream reports in chronic PTSD. Depress Anxiety . 1999;9:146-148.
22. Bartzokis G, Lu PH, Turner J, et al. Adjunctive risperidone in the treatment of combat-related posttraumatic stress disorder. Biol Psychiatry. 2005;57:474-479.
23. Monnelly EP, Ciraulo DA, Knapp C, Keane T. Low-dose risperidone as adjunctive therapy for irritable aggression in posttraumatic stress disorder. J Clin Psychopharmacol. 2003;23:193-196.
24. Pivac N, Kozaric-Kovacic D, Muck-Seler D. Olanzapine versus fluphenazine in an open trial in patients with psychotic combat-related post-traumatic stress disorder. Psychopharmacol (Berl.)2004;175:451-456.
25. Petty F, Brannan S, Casada J, et al. Olanzapine treatment for post-traumatic stress disorder: an open-label study. Int Clin Psychopharmacol. 2001;16:331-337.
26. Hamner MB, Deitsch SE, Brodrick PS, et al. Quetiapine treatment in patients with posttraumatic stress disorder: an open trial of adjunctive therapy. J Clin Psychopharmacol. 2003;23:15-20.
27. Siddiqui Z, Marcil WA, Bhatia SC, et al. Ziprasidone therapy for post-traumatic stress disorder. J Psychiatry Neurosci. 2005;30:430-431.Ü
28. Lambert MT. Aripiprazole in the management of post-traumatic stress disorder symptoms in returning Global War on Terrorism veterans. Int Clin Psychopharmacol. 2006;21:185-187.
29. Pivac N, Kozaric-Kovacic D. Pharmacotherapy of treatment-resistant combat-related posttraumatic stress disorder with psychotic features. Croat Med J. 2006;47:440-451.
30. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27:596-601.
31. Braun P, Greenberg D, et al. Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry. 1990;51:236-238.
32. Mellman TA, Byers PM, Augenstein JS. Pilot evaluation of hypnotic medication during acute traumatic stress response. J Trauma Stress. 1998;11:563-569.
33. Gelpin E, Bonne O, Peri T, et al. Treatment of recent trauma survivors with benzodiazepines: a prospective study. J Clin Psychiatry. 1996;57:390-394.
34. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44:56-63.
35. Pitman RK, Delahanty DL. Conceptually driven pharmacologic approaches to acute trauma. CNS Spectr . 2005;10:99-106.
36. Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160:371-373.
37. Taylor FB, Lowe K, Thompson C, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59:577-581.
38. Vaiva G, Ducrocq F, Jezequel K, et al. Immediate treatment with propranolol decreases posttraumatic stress disorder two months after trauma. Biol Psychiatry. 2003;54:947-949.
39. Pittman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Biol Psychiatry. 2002;15:189-192.
40. Lipper S, Davidson JRT, Grade TA, et al. Preliminary study of carbamazepine in post-traumatic stress disorder. Psychosomatics. 1986;27:849-854.
41. Fesler FA. Valproate in combat-related posttraumatic stress disorder. J Clin Psychiatry. 1991;52:361-364.
42. Berlant J, van Kammen DP. Open-label topiramate as primary or adjunctive therapy in chronic civilian posttraumatic stress disorder: a preliminary report. J Clin Psychiatry. 2002;63:15-20.
43. Hammer MB, Brodrick PS, Labbate LA. Gabapentin in PTSD: a retrospective, clinical series of adjunctive therapy. Ann Clin Psychiatry. 2001;13:141-146.
44. Hertzberg MA, Butterfield MI, Feldman ME, et al. A preliminary study of lamotrigine for the treatment of posttraumatic stress disorder. Biol Psychiatry. 1999;45:1226-1229.
To comment on this article, contact editor@uspharmacist.com.






