US Pharm. 2008;33(7):HS12-HS15.
The human body responds to
injury and infection by a process called inflammation. During an inflammatory
process in the body, the levels of C-reactive protein (CRP), a
pro-inflammatory cytokine, rise dramatically. It has been suggested that
testing CRP levels in the blood may be an additional way to assess
cardiovascular disease risk. Laboratory findings from clinical and research
studies also suggest that inflammation is an important factor in
atherosclerosis. This is the process in which fatty deposits build up in the
inner lining of arteries.1
The American Heart Association
and the Centers for Disease Control and Prevention published a joint
scientific statement in 2003 on the use of inflammatory markers in clinical
and public health practice.2 This statement was developed after
systematically reviewing the evidence of association between inflammatory
markers (mainly CRP) and coronary heart disease and stroke. A more sensitive
CRP test, called a high-sensitivity C-reactive protein (hs-CRP) assay,
is available to determine heart disease risk more accurately.1
In 1930, Tillett and Francis
originally discovered CRP as a substance in the serum of patients with acute
inflammation that reacted with the C-polysaccharide of pneumococcus. Initially,
it was thought that CRP might have a pathogenic role, as it was elevated in
people with a variety of illnesses, but discovery of its hepatic synthesis and
secretion closed that debate. Measuring and charting CRP values can prove
useful in determining disease progression or the effectiveness of treatments.
CRP is used mainly as a marker of inflammation.3
Various analytic methods are
available for CRP determination, such as enzyme-linked immunosorbent assay
(ELISA), immunoturbidimetry, rapid immunodiffusion, and visual agglutination.
In general, both the CRP test and another test, called the erythrocyte
sedimentation rate (ESR), measure the increase in inflammatory generated
proteins. The CRP test is a direct measurement of C-reactive protein, while
ESR indirectly measures many proteins associated with inflammation.1
Causes of Inflammation
There are many
conditions that cause inflammation. Genetics play a role, as does the
environment. Environmental factors include diet, exposure to toxins, germs,
pollutants, and inhalants. Some people have a genetic predisposition to
increased inflammation, which can cause them to develop an illness such as
rheumatoid arthritis.4,5
Acute inflammation is a
complex biological response of vascular tissues to harmful stimuli, such as
pathogens, damaged cells, or irritants. It is a protective attempt by the body
to remove the injurious stimuli as well as to initiate the healing process for
the tissue. Chronic inflammation is a pathologic condition characterized by
concurrent active inflammation, tissue degeneration, and attempts at repair.
Chronic inflammation is not characterized by the classic signs of acute
inflammation (i.e., swelling, redness, pain, heat, loss of function). Instead,
chronically inflamed tissue is characterized by the infiltration of
mononuclear immune cells (i.e., monocytes, macrophages, lymphocytes, plasma
cells) and tissue destruction, which include angiogenesis and fibrosis.
Cigarette smoking,
hypertension, atherogenic lipoproteins, and hyperglycemia are well-established
promoting factors in atherogenesis. These risk factors give rise to a variety
of noxious stimuli that cause the release of certain chemicals and the
activation of cells involved in the inflammatory process. These events are
thought to contribute not only to the formation of plaque but may also
contribute to its disruption, resulting in the formation of a blood clot.
Thus, virtually every step in atherogenesis is believed to involve substances
involved in the inflammatory response and cells that are characteristic of
inflammation.6
In addition, there is research
that indicates that an infection--possibly one caused by a bacterium or a
virus--might contribute to or even cause atherosclerosis.7 The
infectious bacterium Chlamydia pneumoniae has been shown to have a role
in atherosclerotic plaque. The herpes simplex virus has also been proposed as
an initial inflammatory infectious agent in atherosclerosis. Viral infections
tend to give a lower CRP level than bacterial infection. Bacterial infection
with Helicobacter pylori is now known to be the major cause of
inflammatory stomach lesions. The treatment for this condition routinely
includes antibiotic therapy.
In diseases such as allergies,
anemia, arthritis, fibromyalgia, fibrosis, heart attack, aortic valve
stenosis, kidney failure, lupus, pancreatitis, and psoriasis, the levels of
inflammatory cytokines are elevated, which induces damage to the tissues. In
surgical complications, the inflammatory cytokines prevent healing.
CRP and New Cardiovascular
Events
Scientific studies
have found that the higher the hs-CRP levels, the higher the risk of having a
heart attack. In fact, the risk for heart attack in people with high hs-CRP
levels has been determined to be twice that of those whose hs-CRP levels are
lower. These prospective studies included men, women, and the elderly. Studies
have also found an association between sudden cardiac death, peripheral
arterial disease, and high hs-CRP levels. However, not all of the established
cardiovascular risk factors were controlled for when the association was
examined. The true independent association between hs-CRP and new
cardiovascular events has yet to be established.8
CRP and Recurrent Events
A growing number of
studies have examined whether high hs-CRP levels can predict recurrent
cardiovascular disease, stroke, and death in different settings. High levels
of hs-CRP consistently predict recurrent coronary events in patients with
unstable angina and acute myocardial infarction (heart attack). Higher hs-CRP
levels also are associated with lower survival rates in these patients. Many
studies have suggested that after adjusting for other prognostic factors,
hs-CRP is useful as a risk predictor.8
Studies also suggest that
higher levels of hs-CRP may increase the risk that an artery will reclose
after it has been opened by balloon angioplasty. High levels of hs-CRP in the
blood also seem to predict prognosis and recurrent events in patients with
stroke or peripheral arterial disease. CRP inhibition can be a safe and
effective therapy for myocardial and cerebral infarctions.8
When to Measure CRP
If a person's
cardiovascular risk factors (i.e., smoking, hypertension, high blood
cholesterol, diabetes, being overweight or obese, physical inactivity) are
low, the possibility of developing cardiovascular disease is less than 10% in
10 years, and no test is immediately warranted. If the risk factors are in the
intermediate range, the possibility is 10% to 20% in 10 years, and such a test
can help predict a cardiovascular or stroke event as well as help direct
further evaluation and therapy. However, the benefits of therapy based on this
strategy remain uncertain. A person with a high-risk score (>20% in 10 years)
or established heart disease or stroke should be treated intensively
regardless of hs-CRP levels.9
Diagnostic Criteria
As previously
mentioned, CRP is used mainly as a marker of inflammation. Measuring and
charting CRP values can prove useful in determining cardiovascular and
noncardiovascular disease progress or the effectiveness of treatments. Blood
samples are analyzed in a medical laboratory or at the point of testing.
Patients who are scheduled for a CRP test will be asked not to eat or drink
anything for 12 hours before the test.
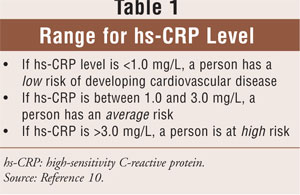
The ranges for evaluating hs-CRP levels are
given in Table 1. If, after repeated testing, patients have
persistently unexplained, markedly elevated hs-CRP levels (>10.0 mg/L), they
should be evaluated to exclude noncardiovascular causes. Patients with
autoimmune diseases or cancer, as well as other infectious diseases, may also
have elevated CRP levels.10
Mode of Action
The CRP gene is
located on the first chromosome and is a 224-residue protein with a monomer
molar mass of 25106 dalton. The protein is an annular pentameric disk in
shape. Proteins with this type of configuration are known as pentraxins.
CRP binds to phosphorylcholine on microbes. It is thought to assist in
complement binding to foreign and damaged cells, and it enhances phagocytosis
by macrophages, which express a receptor for CRP. It is also believed to play
an important role in innate immunity, as an early defense system against
infections.11
Arterial damage is thought to
result from inflammation due to chemical insults. CRP can be used as a marker
for the extent of this damage, but by itself it is not a specific prognostic
indicator. Clinicians only look at the CRP values with prolonged elevation, so
a single measurement would be meaningless.
In different disease states,
one or two amino acids get "lopped off" CRP. It retains its activity, but
these losses open it up to glycosylation, and it may have sugars such as
glucose, galactose, and mannose attached to it. The patterns of glycosylation
vary in different diseases, but are similar among patients who have the same
disease. Previous work has shown that CRP increased the rate at which a
particular parasite could invade blood cells.12 The study showed
that the various CRPs had very different potencies in this regard. The authors
speculate that subtyping CRP may give us more insight into heart attack
mechanisms. Although the study did not demonstrate whether this glycosylation
of CRP was a "good" or a "bad" thing, it offered circumstantial evidence that
the differing glycosylation is part of CRP's mode of action.12
The Role of CRP in Cancer
The role of
inflammation in cancer is well known. Some organs of the body show greater
risk of cancer when they are chronically inflamed. Blood samples of persons
with colon cancer have an average CRP concentration of 2.69 mg/L. Persons
without colon cancer average 1.97 mg/L. The difference was statistically
significant (P <.001).13 These findings concur with
previous studies that indicated that anti-inflammatory drugs could lower colon
cancer risk.14
Pharmacist Recommendation
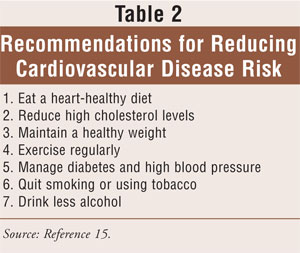
It is important for
patients to make lifestyle changes to reduce their risk for cardiovascular
disease, especially if the CRP level is intermediate or high (Table 2).15
For those with an elevated CRP level, taking aspirin may provide protection
from cardiovascular disease. Statins, the most commonly prescribed drugs for
lowering cholesterol, may also reduce CRP levels. Clinicians should prescribe
the correct medications and dosage to treat the disease condition.
REFERENCES
1. Danesh J,
Wheeler JG, Hirschfield GM, et al. C-reactive protein and other circulating
markers of inflammation in the prediction of coronary heart disease. N Engl
J Med. 2004;350:1387-1397.
2. Ford ES. C-reactive protein concentration and cardiovascular disease risk factor in children: findings from the National Health and Nutrition Examination Survey 1999-2000. Circulation. 2003;106:1053-1058.
3. Tillett WS, Francis Jr T. Serological reactions in pneumonia with a nonprotein somatic fraction of pneumococcus. J Exp Med. 1930;52:561-585.
4. West SG. Rheumatology Secrets. 2nd ed. Philadelphia, PA: Hanley & Belfus; 2002:54.
5. Dehghan A, van Hoek M, Sijbrands EJ, et al. Genetic variation, C-reactive protein levels, and incidence of diabetes. Diabetes. 2007:56:872-878.
6. Lau DC, Dhillon B, Yan H, et al. Adipokines: molecular links between obesity and atherosclerosis. Am J Physiol Heart Circ Physiol. 2005;288:H2031-H2041.
7. Burke AP, Tracy RP, Kolodgie F, et al. Elevated C-reactive protein values and atherosclerosis in sudden coronary death. Circulation. 2002;105:2019-2023.
8. Abdelmouttaleb I, Danchin N, Ilardo C, et al. C-reactive protein and coronary artery disease: additional evidence of the implication of an inflammatory process in acute coronary syndromes. Am Heart J. 1999;137:346-351.
9. Pradhan AD, Manson JE, Rifai N, et al. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA. 2001;286:327-334.
10. Pepys MB, Hirschfield GM, Tennent GA, et al. Targeting C-reactive protein for the treatment of cardiovascular disease. Nature. 2006;440:1217-1221.
11. Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111:1805-1812.
12. Das T, Sen AK, Kempf T, et al. Induction of glycosylation in human C-reactive protein under different pathological conditions. Biochem J. 2003;373:345-355.
13. Erlinger TP, Platz EA, Rifai N, Helzlsouer KJ. C-reactive protein and the risk of incident colorectal cancer. JAMA. 2004;291:585-590.
14. Baron JA, Cole BF, Sandler RS, et al. A randomized trial of aspirin to prevent colorectal adenomas. N Engl J Med. 2003;348:891-899.
15. Lopez-Garcia E, Schulze MB,
Meigs JB, et al. Consumption of trans fatty acids is related to plasma
biomarkers of inflammation and endothelial dysfunction. J Nutr.
2005;135:562-566.
To comment on this article, contact rdavidson@jobson.com.





