US Pharm. 2008;33(1):38-45.
Obtaining the knowledge and
skills required to perform disease-prevention patient interventions is
becoming increasingly more important for pharmacists and other health care
professionals. The overall health of almost all populations appears to be
better if diseases are prevented rather than treated once they occur. Chronic
diseases create a significant burden upon the U.S. health care system at a
societal and personal level as well as from a financial standpoint. The
Centers for Disease Control and Prevention (CDC) reports that 70% of the
deaths of all Americans and 75% of the annual health care costs in the U.S.
are related to chronic diseases.1 These data indicate that a focus
on the prevention of these chronic diseases may produce better overall
outcomes for patients and be cost effective for the U.S. health care system.
Pharmacists have long been
known to be highly accessible and trusted health care providers. They have
frequent contact with patients who could potentially benefit from
lifestyle-modification education. Pharmacists are, therefore, in an ideal
position to offer patients information, guidance, and counseling regarding
lifestyle changes that can help manage their medical conditions. Training
student pharmacists to become proficient with the knowledge and skills to
educate patients about lifestyle-modification strategies may decrease the
burdens that chronic diseases impose on the U.S. health care system and is
justifiable for several other reasons as well. The purpose of this article is
to provide justification for why student and practicing pharmacists should be
trained to educate and treat patients using lifestyle-modification strategies.
Educating Health Care
Practitioners
Preventing and
treating chronic diseases through lifestyle modifications is becoming an
important aspect of patient-care regimens. As a result, educating and training
health care practitioners with the proper skills needed to care for patients
through the use of lifestyle modifications is now becoming an important issue
in health professions education. In 2003, the Institute of Medicine (IOM)
published a report outlining its recommendations for educating students in the
health professions.2 The recommendations describe the need for all
programs that educate health care professionals to integrate five core
competencies. One of the five core competencies includes delivering
patient-centered care, described as a type of care that continuously advocates
for disease prevention, wellness, and the promotion of healthy lifestyles.
2
Pharmacy-specific educational
recommendations have also been proposed. In 2004, the American Association of
Colleges of Pharmacy's (AACP) Center for the Advancement of Pharmaceutical
Education (CAPE) released its Educational Outcomes.3 The major
recommendations of the 2004 Educational Outcomes include an emphasis on
pharmaceutical care, systems management, and public health.3 The
public health component is intended to promote health improvement, wellness,
and disease prevention.3
Also in 2004, the National
Association of Boards of Pharmacy (NABP) released new blueprint standards for
the North American Pharmacist Licensure Examination (NAPLEX).4
Competency 3.2.2 states: "Provide health care information regarding nutrition,
lifestyle, and other non-drug measures that are effective in promoting health
or preventing or minimizing the progression of a disease or medical condition."
4 Both the CAPE Educational Outcomes and the NAPLEX blueprint standards
are important documents for pharmacy programs to consider when educating
students.
Organizations outside of
higher education have also stressed the importance of lifestyle modifications
for improving overall health. Healthy People 2010 (sponsored by the U.S.
Department of Health and Human Services) is a set of health objectives for the
U.S. to achieve over the first decade of the century.5 The
objectives focus on 28 major areas that were developed by leading federal
agencies with the most relevant scientific expertise. Ten Leading Health
Indicators (LHI) are identified in Healthy People 2010 that reflect the major
health concerns in the U.S. at the beginning of the 21st century.5
The top three LHI include physical activity, overweight and obesity, and
tobacco use, all of which are lifestyle behaviors.
In 2002, the Healthy People
Curriculum Task Force was established by the Association of Prevention
Teaching and Research (APTR) and the Association for Academic Health Centers
(AHC) as a multidisciplinary group of seven health professions disciplines,
including pharmacy.6 Its mission is to fulfill the Healthy People
2010 Objective 1.7, which states: "Increase the proportion of schools of
medicine, schools of nursing and health professional training schools whose
basic curriculum for health care providers includes the core competencies in
health promotion and disease prevention."6 The curricular
framework outlined by the task force includes the areas of evidence-based
practice, clinical preventive services, health promotion, health systems and
health policy, and community aspects of practice. It is recommended that each
health profession (i.e., pharmacy) adapt the curricular framework to meet the
needs of its discipline.6
Leading Versus Actual
Causes of Death
Many times, health
care professionals and the public tend to focus on the leading causes of death
as a benchmark for the diseases that should receive more attention when
treating patients and considering population health matters. Certainly, the
U.S. health care system adequately directs resources and attention to these
leading causes of death. However, consideration should also be given to
addressing the actual reasons why individuals die from a certain disease or
circumstance. For example, heart disease has been the leading cause of death
for several decades. Among the most common reasons that Americans develop
heart disease are related to conditions such as hypertension, dyslipidemia,
and diabetes mellitus.7,8 Taking this one step further, among the
most common reasons that individuals develop these conditions are tobacco use,
poor nutrition, physical inactivity, and obesity.7,8 Therefore,
greater resources and attention should be placed on controlling the risk
factors that can ultimately prevent the final death outcomes, such as
lifestyle-related behaviors.
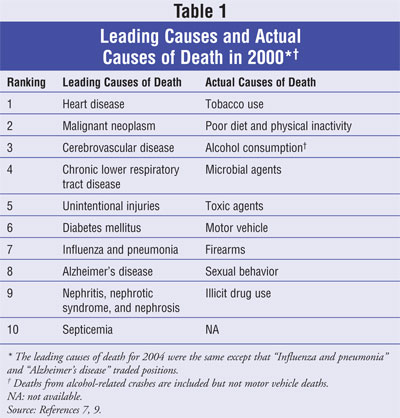
In 2004, Mokdad et al from the
CDC published a study listing not only the leading causes of death from 2000
but the actual causes as well.7,8 The top three leading causes of
death in 2000 were heart disease, cancer, and stroke. The top three reasons
why individuals died from these diseases, however, were tobacco use, poor diet
and physical inactivity, and alcohol consumption. Therefore, even though heart
disease, cancer, and stroke are the most prevalent reasons for death in
America, they result from lifestyle behaviors that can be modified in many
individuals.7,8 The leading causes of death and actual causes of
death from the year 2000 are listed in TABLE 1.7,9
Treatment Guidelines
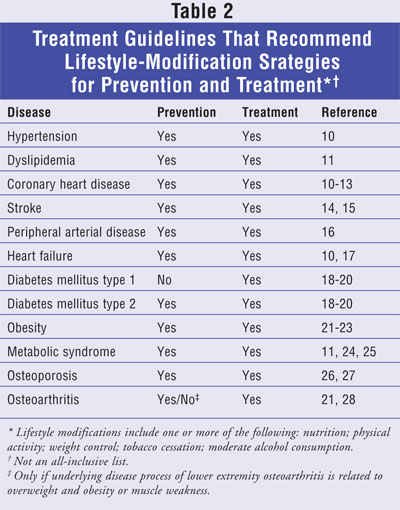
Because lifestyle
behaviors have been shown to be effective in preventing and treating several
types of diseases that can ultimately lead to a high prevalence of morbidity
and mortality, several widely accepted treatment guidelines for specific
diseases include lifestyle-modification strategies. The lifestyle-modification
strategies that are most commonly recommended within treatment guidelines
include proper nutrition, physical activity, weight control, tobacco
cessation, alcohol moderation, and health behaviorñchange strategies. Several
diseases are listed in TABLE 2 in which the treatment guideline for
that disease recommends lifestyle-modification strategies as part of its
treatment and prevention regimen.
Pharmacy Practice
Application
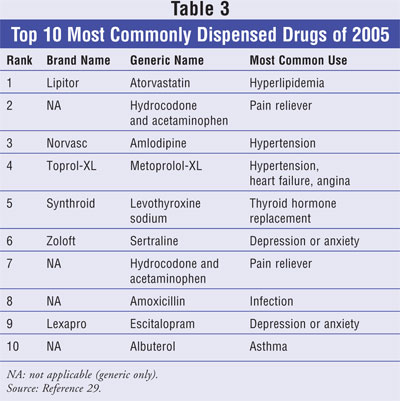
When looking at the
drugs that are most commonly dispensed in a pharmacy setting, it is easy to
see that many of these medications treat conditions in which lifestyle
modifications are recommended for treatment and prevention. An analysis of the
top 200 drugs by prescription count in 2005 shows that 31% (62/200) of these
drugs are prescribed for the medical conditions of hyperlipidemia,
hypertension, glycemic control, osteoporosis, or osteoarthritis.29
As shown in TABLE 2, the treatment guidelines for each of these
conditions recommend one or more lifestyle-modification strategies. Therefore,
if pharmacists are truly practicing pharmaceutical care and medication therapy
management (MTM), lifestyle-change behaviors should be incorporated in the
patients care plan along with appropriate drug therapy and drug therapy
counseling. The 10 most commonly dispensed drugs of 2005, with their primary
indication, are listed in TABLE 3.29
When looking at the U.S. adult
population health-behavior data, it is also easy to see that a great need
exists for pharmacists and other health care professionals to educate the
general public about lifestyle behaviors. From 2003 to 2004, an estimated 66%
of the U.S. adult population was considered overweight or obese and nearly 21%
of adults were active cigarette smokers.30,31 Additionally, in
2005, 52% of U.S. adults were physically inactive or engaged in insufficient
amounts of physical activity.32 That same year, more than 76% of
U.S. adults did not consume the recommended amounts of daily fruits and
vegetables.33 These data show that a large percentage of the
general population could benefit from lifestyle-modification interventions
that could be offered by pharmacists and other health care professionals.
Discussion
Incorporating
lifestyle-modification patient care into the practice of pharmacy requires an
increased educational focus in this area on the part of both practicing
pharmacists and student pharmacists. Practicing pharmacists can obtain
education and training through continuing education credits, and students can
gain the knowledge and skills as part of their pharmacy curriculum. One of the
current limitations for students to obtain this type of training may be the
lack of opportunities that pharmacy schools currently offer their students or
the fact that students may not be aware that pharmacists can be well suited to
offer their patients this type of information.
In order to assess student
pharmacists' beliefs, interests and perceptions about pharmacists offering
lifestyle-modification services to patients, the Creighton University School
of Pharmacy and Health Professions recently conducted a survey. As part of a
special project, a third-year pharmacy student delivered a presentation to the
student pharmacists at Creighton on the topic of lifestyle-modification
education in pharmacy schools. Following the presentation, the students who
attended were asked to complete a survey with the purpose of obtaining 1)
student beliefs about counseling patients on lifestyle-modification topics in
pharmacy practice; 2) student perceptions of pharmacists' qualifications to
counsel patients on lifestyle-modification topics; and 3) student interest in
learning more about lifestyle-modification topics. For the purposes of the
survey, lifestyle-modification topics were defined as physical activity,
nutrition, weight control, and smoking cessation.
A total of 38 students
attended the presentation and all 38 completed the survey. Fifty-five percent
of the students were in their third year of pharmacy school, while 16% and 29%
were in their second and first years, respectively. Seventy-six percent of the
survey participants were female.
The results of the survey
showed that all students who attended (38/38) believe that
lifestyle-modification counseling should be part of the overall care plan for
patients and 89% (34/38) felt that it was part of the duties of a pharmacist
to offer lifestyle-modification counseling to patients. Most of the students
(54%, 20/37) felt that pharmacists are qualified or very qualified to counsel
patients on lifestyle modifications. Additionally, 97% (37/38) would like to
receive more training on smoking cessation and weight control, and 95% (36/38)
would like to receive more training on implementing physical activity and
nutrition strategies into a patient's care plan. Lastly, 100% (38/38) of the
attendants would like a greater overall focus on lifestyle-modification
training in the pharmacy curriculum at Creighton.
The major limitation to this
survey was that participation was not mandatory for the entire student body.
Therefore, it is likely that those students who attended the presentation were
interested in the topic, making it difficult to generalize the results to all
students. Nonetheless, all students who attended the presentation participated
in the survey and overwhelming expressed a very high interest in incorporating
lifestyle modification strategies into patient care. Such information is
encouraging and should prompt pharmacy schools to considering offering courses
that include this type of patient care, not only because many national
organizations state that they should, but because there may also be high
student interest as well.
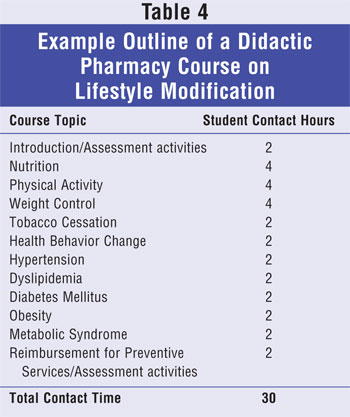
Recently, the Creighton
University School of Pharmacy and Health Professions began teaching an
elective course designed to train student pharmacists about
lifestyle-modification strategies in conjunction with medication therapy. The
course objectives are to educate students about proper nutrition, physical
activity, weight control, tobacco cessation, and health-behavior change
strategies. Students spend approximately half of the course time applying
these strategies to sample case patients with diseases such as hypertension,
dyslipidemia, diabetes mellitus, obesity, and metabolic syndrome. The course
topics and allotted number of student contact hours for the 15-week semester
are listed in TABLE 4. Other diseases could also be incorporated into
the course, such as coronary heart disease, stroke, peripheral arterial
disease, heart failure, cancer, osteoporosis, and osteoarthritis. The course
places a major emphasis on developing wellness prescriptions that are designed
to work in conjunction with a patient's existing drug therapy regimen to
either prevent disease or more effectively manage existing disease. Courses
such as this could be incorporated at other schools and colleges of pharmacy
to help meet recommendations for training students to promote health and
prevent disease. Likewise, continuing education programs with this same design
could be offered to practicing pharmacists to improve their skills in
counseling patients about lifestyle modifications.
The American Pharmacists
Association (APhA) Foundation has sponsored several projects to show that
lifestyle-modification strategies can be incorporated into pharmacy practice
settings.34-40 These projects have focused on treating diseases
such as hyperlipidemia, osteoporosis, diabetes mellitus, and asthma.34-40
Results from these studies show that incorporating lifestyle-modification
strategies into pharmacy practice settings can logistically be accomplished,
improve patient outcomes, and are reimbursable and cost effective.34-40
Training student and practicing pharmacists to acquire the skills necessary
to perform this type of care should begin in the pharmacy schools and be given
through continuing education sessions for practicing pharmacists. This would
give pharmacists greater opportunities to practice clinical patient care and
receive reimbursement for doing so.
Conclusions
Pharmacists are in
an ideal position within the community to offer lifestyle-modification
counseling to patients with the purpose of preventing and/or controlling
disease, but they must receive adequate training in order to do so. The
sections described in this article outline several reasons why pharmacy
schools should incorporate lifestyle-modification strategies as a component of
their curriculum and offer practicing pharmacists more opportunities to obtain
knowledge and skills related to lifestyle-modification counseling. Many higher
education organizations, both in and outside of pharmacy, recommend that
student pharmacists receive training on these topics. Additionally, if
pharmacy schools are training their students to practice high-quality
pharmaceutical care and MTM, lifestyle-modification strategies should be part
of the overall treatment plan according to many disease-treatment guidelines.
Pharmacists are in regular contact with patients who could benefit from
lifestyle-modification interventions simply by the prescriptions they dispense
and by the proportion of the general public with whom they are in contact and
who could benefit from these strategies. The aggregate of this information
indicates that pharmacy schools should consider ways in which to incorporate
lifestyle-modification strategies into their current curricula to decrease the
burdens that chronic diseases impose on the U.S. health care system.
References
1. Department of
Health and Human Services. Centers for Disease Control and Prevention. Chronic
Disease Prevention. At a Glance 2007. Available at:
www.cdc.gov/nccdphp/publications/AAG/steps.htm. Accessed May 9, 2007.
2. Greiner AC, Knebel
E, eds. Health Professions Education: A Bridge to Quality. Executive Summary
. Institute of Medicine of the National Academies. Washington, DC: The
National Academies Press; 2003:3-4.
3. Educational Outcomes
2004. American Association of Colleges of Pharmacy. Center for the Advancement
of Pharmaceutical Education. Available at:
www.aacp.org/Docs/MainNavigation/Resources/ 6075_CAPE2004.pdf. Accessed May 9,
2007.
4. NAPLEX Blueprint.
The NAPLEX Competency Statements. Available at:
www.nabp.net/ftpfiles/NABP01/updatednaplexblueprint.pdf. Accessed
May 9, 2007.
5. Healthy People 2010,
Office of Disease Prevention and Health Promotion, U.S. Department of Health
and Human Services. Available at: www.healthypeople.gov. Accessed May 9, 2007.
6. Healthy People
Curriculum Task Force, Association of Prevention Teaching and Research.
Available at: www.aptrweb.org/taskforce/ HPC_Taskforce.html. AccessedÜ May 9,
2007.
7. Mokdad AH, Marks JS,
et al. Actual causes of death in the United States, 2000. JAMA.
2004;291:1238-1245.
8. Mokdad AH.
Correction: actual causes of death in the United States, 2000. JAMA.
2005;293:293-294.
9. Minino AM, Heron MP,
Smith BL. U.S. Department of Health and Human Services, Centers for Disease
Control and Prevention, National Center for Health Statistics. National Vital
Statistics System. Nat Vit Stat Rep. 2006;54:30.
10. Chobanian AV,
Bakris GL, et al. Seventh report of the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Hypertension. 2003;42:1206-1252.
11. National Institutes
of Health, National Heart, Lung, and Blood Institute. Third report of the
National Cholesterol Education Program (NCEP) expert panel on detection,
evaluation, and treatment of high blood cholesterol in adults (Adult Treatment
Panel III). NIH Publication No. 02-5215. September 2002.
12. HHS Publication
number: HHS-ODPHP-2005-01-DGA-A, Dietary Guidelines for Americans 2005, United
States Department of Health and Human Services, United States Department of
Agriculture. Available at: http://healthierus.gov/dietaryguidelines. Accessed
May 9, 2007.
13. U.S. Department of
Agriculture and U.S. Department of Health and Human Services. Nutrition and
Your Health: Dietary Guidelines for Americans, 5th ed. Home and Garden
Bulletin No. 232. Washington, DC: U.S. Department of Agriculture, 2000.
14. Goldstein LB, Adams
R, et al. AHA Scientific Statement. Primary prevention of ischemic stroke: a
statement for healthcare professionals from the Stroke Council of the American
Heart Association. Circulation. 2001;103:163-182.
15. Gordon NF, Gulanick
M, et al. AHA Scientific Statement. Physical activity and exercise
recommendations for stroke survivors. Circulation. 2004;109:2031-2041.
16. Hirsch AT, Haskal
ZJ, et al. ACC/AHA guidelines for the management of patients with peripheral
arterial disease (lower extremity, renal, mesenteric, and abdominal aortic):
executive summary: a report of the American College of Cardiology/American
Heart Association Task Force on Practice Guidelines (Writing Committee to
Develop Guidelines for the Management of Patients With Peripheral Arterial
Disease [Lower Extremity, Renal, Mesenteric, and Abdominal Aortic]). J Am
Coll Cardiol. 2006;47:1239-1312.
17. Hunt SA, Abraham
WT, et al. ACC/AHA 2005 guideline update for the diagnosis and management of
chronic heart failure in the adult: a report of the American College of
Cardiology/American Heart Association Task Force on Practice Guidelines
(Writing Committee to Update the 2001 Guidelines for the Evaluation and
Management of Heart Failure). American College of Cardiology Web site.
Available at: www.acc.org/clinical/guidelines/failure//index.pdf. Accessed May
9, 2007.
18. American Diabetes
Association. Position Statement. Standards of medical care in diabetes--2006.
Diabetes Care. 2006;29(suppl 1):S4-S42.
19. American Diabetes
Association. Position Statement. Nutrition principles and recommendations in
diabetes. Diabetes Care. 2004;27(suppl 1):S36-S46.
20. Feld S. The
American Association of Clinical Endocrinologists medical guidelines for the
management of diabetes mellitus: the AACE system of intensive diabetes
self-management--2002 update. Endocrine Practice. 2002;8(suppl
1):40-82.
21. Clinical Guidelines
on the Identification, Evaluation, and Treatment of Overweight and Obesity in
Adults. Bethesda, MD: National Institutes of Health, U.S. Department of Health
and Human Services; 1998. NIH Publication No. 98-4083.
22. The Practical
Guide. Identification, Evaluation, and Treatment of Overweight and Obesity in
Adults. Bethesda, MD: National Institutes of Health, U.S. Department of
Health and Human Services; 2000. NIH Publication No. 00-4084.
23. ACSM position stand
on the appropriate intervention strategies for weight loss and prevention of
weight regain for adults. Med Sci Sports Exerc. 2001;33:2145-2156.
24. Grundy SM, Cleeman
JI, et al. Diagnosis and management of the metabolic syndrome. An American
Heart Association/National Heart, Lung, and Blood Institute scientific
statement: executive summary. Circulation. 2005;112:1-6.
25. Khan R, Buse J, et
al. The metabolic syndrome: time for a critical appraisal. Joint statement
from the American Diabetes Association and the European Association for the
Studies of Diabetes. Diabetes Care. 2005;28:2289-2304.
26. U.S. Department of
Health and Human Services. Bone Health and Osteoporosis: A Report of the
Surgeon General. Rockville, MD: U.S. Department of Health and Human Services,
Office of the Surgeon General; 2004.
27. Kohrt WM,
Bloomfield SA, et al. American College of Sports Medicine: position stand:
physical activity and bone health. Medicine and Science in Sports and
Exercise. 2004;36:1985-1996.
28. Messier SP.
Arthritic disease and conditions. Kaminsky LA, et al, eds. In: ACSM's
Resource Manual for Guidelines for Exercise Testing and Prescription. 5th
ed. Baltimore, MD: Lippincott, Williams and Wilkins; 2006:500-513.
29. Pharmacy Times Top
200 Prescription Drugs of 2005. Available at:
www.nationaltechexam.org/pdf/top_200_drug_list05.pdf. Accessed May 9, 2007.
30. Department of
Health and Human Services. Centers for Disease Control and Prevention.
National Center for Health Statistics. Prevalence of overweight and obesity
among adults: United States, 2003-2004. Available at:
www.cdc.gov/nchs/products/pubs/pubd/hestats/overweight/ overwght_adult_03.htm.
Accessed May 9, 2007.
31. Department of
Health and Human Services. Centers for Disease Control and Prevention. Smoking
and tobacco use. Available at:
www.cdc.gov/tobacco/data_statistics/tables/adult/table_2.htm. Accessed
May 9, 2007.
32. Department of
Health and Human Services. Centers for Disease Control and Prevention.
Behavioral Risk Factor Surveillance System (BRFSS), 2005. U.S. physical
activity statistics. Available at:
http://www.cdc.gov/nccdphp/dnpa/physical/stats/index.htm. Accessed
May 9, 2007.
33. Department of
Health and Human Services. Centers for Disease Control and Prevention. Fruit
and vegetable consumption data statistics. Available at:
http://apps.nccd.cdc.gov/5ADaySurveillance. Accessed May 9, 2007.
34. American
Pharmacists Association Foundation. Available at: www.aphafoundation.org.
Accessed May 9, 2007.
35. Bluml BM, McKenney
JM, Cziraky MJ. Pharmaceutical care services and results in Project ImPACT:
hyperlipidemia. J Am Pharm Assoc. 2000;40:157-165.
36. Goode JV, Swiger K,
Bluml BM. Regional osteoporosis screening, referral, and monitoring program in
community pharmacies: findings from Project ImPACT: osteoporosis. J Am
Pharm Assoc. 2004;44:152-160.
37. Cranor CW, Bunting
BA, Christensen DB. The Asheville Project: long-term clinical and economic
outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc
. 2003;43:173-184.
38. Garrett DG, Martin
LA. The Asheville Project: Participants' perceptions of factors contributing
to the success of a patient self-management diabetes program. J Am Pharm
Assoc. 2003;43:185-190.
39. Garrett DG, Bluml
BM. Patient self-management program for diabetes: first-year clinical,
humanistic, and economic outcomes. J Am Pharm Assoc. 2005;45:130-137.
40. Bunting BA, Cranor
CW. The Asheville Project: long-term clinical, humanistic, and economic
outcomes of a community-based medication therapy management program for asthma
. J Am Pharm Assoc. 2006;46:133-147.
To comment on this article, contact
editor@uspharmacist.com.





