US Pharm.
2007;32(10)(Oncology suppl):1-8.
The post-test exam and post-activity
evaluation form are available at www.cmeuniversity.com.
Patient adherence with many long-term drug
therapies to manage chronic illness is low. Until recently, patient adherence
to antineoplastic therapy was relatively unaddressed because most cancer
therapies were delivered intravenously. Although oral antineoplastic therapies
offer patients many advantages, including greater convenience, less time away
from work and family, increased independence, and the potential for attenuated
adverse effects compared with traditional therapies, patient adherence to oral
agents is more difficult to assess than adherence to intravenous (IV)
medications and is relatively unstudied.1,2 In fact, patient
nonadherence may be the greatest barrier to the effective use of new oral
antineoplastic agents, particularly if health care providers fail to consider
this potential obstacle to treatment.1 Consequently, a greater
focus on adherence among patients using oral antineoplastic agents is
critical.
PATIENT NONADHERENCE IN THE CONTEXT OF
CANCER
Adherence to (or compliance with)
medication is the extent to which patients take medications as prescribed by
their clinicians.3 Adherence may refer to the frequency with which
a patient takes the recommended dose (the prescribed number of pills each day)
and follows prescribing orders that reflect the timing of the dose (the
prescribed time period when the dose should be taken). The word "adherence" is
typically preferred because "compliance" suggests that the patient plays a
passive role that is subordinate to the role of the clinician.4
Regardless of which term is used, the full benefit of medications may not be
realized if patients do not follow their prescribed treatment regimens
relatively closely.3 Despite its importance, adherence is difficult
to objectively measure, monitor, and improve.
Increasing Importance of Adherence in
Cancer Therapy
Historically, the vast majority
of cancer chemotherapy was delivered intravenously.1 New targeted
oral antineoplastic agents that interfere with the molecular and biochemical
pathways causing the malignant phenotype are used increasingly in cancer
therapy.2 The recent increase in the availability and utility of
these oral agents presents new challenges to health care practitioners
involved in medical oncology. Because IV medications are administered with
greater supervision in a more controlled setting than oral formulations,
patient nonadherence to new antineoplastic therapies was rarely of issue.
Adherence with IV therapy was assured as long as patients kept their
appointments for each planned cycle of chemotherapy.2 However,
outcomes are no longer assured, since much of oncology care is now delivered
outside of acute care. Moreover, patients using oral antineoplastic agents may
bypass the pharmacist or nurse who delivers patient education in the
ambulatory setting. Hence, information stressing the importance of following
prescribed dosing instructions, what to do if doses are skipped, and
management of toxicities may not be reinforced.5 The increasing use
of these new oral agents shifts the primary responsibility of ensuring
adherence to patients and their families. However, outcomes from suboptimal
adherence have not been comprehensively addressed.6
Existing Data on Adherence With Antineoplastic Agents
Patient
adherence to oral chemotherapy is
generally assumed not to be a problem due to increased motivation owing to the
gravity of cancer.5 Early studies of patient rigor in following
prescribing directions with oral antineoplastic agents have demonstrated that
adherence to these agents is not necessarily higher than that seen with other
long-term therapies.5-9
Results of available studies are
often contradictory,7 with adherence
estimates ranging from 20% to 100%.6
In one study of outpatients with breast cancer who received 26 weeks of oral
cyclophosphamide, investigators documented a patient self-reported
nonadherence rate of 43%.8 A study of patients with hematologic
malignancies noted
surprisingly low adherence rates with prednisone (27%) and allopurinol (17%).
6,10 More recently, in a 24-month study in which the
prescription-filling rate for imatinib was compared with the clinician's
prescribing rate, the overall adherence rate was 75%.11 Another
study of ambulatory patients found no significant differences between
medication
adherence rates among seriously ill cancer patients receiving chemotherapy,
compared to patients without cancer receiving a variety of drugs for other
chronic illnesses.9
Consequences
of Nonadherence in Medical Oncology
Deficient
adherence to antineoplastic therapy can significantly affect therapeutic
options. In many cases, the degree of patient adherence with oral chemotherapy
can be directly correlated to the treatment's success.5 For
example, studies have demonstrated that insufficient
adherence leading to
underdosing is associated with inferior disease-free survival and compromised
treatment
outcomes.6,12-14 Nonadherence is also linked
with an increased number of
physician visits, higher hospitalization rates, and longer hospitalizations.
6 Suboptimal adherence may also contribute to treatment resistance.2
Additionally, clinicians may attribute a patient's worsening condition or
lack of therapeutic response to the loss or absence of drug activity, which
can result in unnecessary changes in the drug regimen and/or initiation of
unnecessary diagnostic testing. Recent studies have also shown that inadequate
compliance with an oral molecularly targeted antineoplastic agent is
associated with increased total health care and disease-related health care
costs.15
Another type of nonadherence of relevance to oncology patients is the "more is
better" approach. Overadherence to therapy may prevail in the excessive use of
a drug.6 This may stem from a fear that orally formulated
chemotherapy may not be as efficacious as parenterally administered regimens.
This
or the perception that the drug is not acting quickly enough may prompt some
patients to increase doses arbitrarily, which may result in increased drug
toxicity.
BARRIERS TO ADHERENCE WITH
ORAL CHEMOTHERAPIES
Adherence to any long-term intervention is determined largely by the patient's
perception of the risks, benefits, and costs of the intervention.6
Although factors contributing to insubstantial adherence are complex and are
currently not well understood, many barriers to adherence among patients
taking oral antineoplastic agents have been identified (TABLE 1).
3,6,16 These factors can be grouped broadly into logistical, perceptual,
physiologic, and social impediments to treatment.

Logistical Barriers
Particularly in the elderly, adherence to administration schedules can be
directly correlated with regimen complexity. Oral antineoplastics may be
prescribed along with other drug therapies to manage comorbidity requiring
coordination. This complexity is often complicated by consultation with
multiple providers unaware of colleagues' recommendations for drug
consumption. Treatments with a high dosing frequency may have particularly low
rates of adherence. Therapeutic regimens that do not accommodate a patient's
lifestyle or require behavioral changes for optimal adherence, such as dietary
changes, can also be associated with poor adherence, particularly for patients
who travel, have irregular schedules, or have unsupportive family members.
2
Cost constraints may also impede adherence. Out-of-pocket expenses related to
inadequate insurance coverage may cause patients to delay therapy initiation or
decrease dosages to extend medicine
availability.1 Consequently, it is important that health care
providers consider overall treatment costs, insurance coverage, and the
patient's ability to pay when selecting therapies.
The presence of adverse drug effects may
also be associated with reduced adherence.1 The experience of
nausea or vomiting may affect the ability of some patients
to retain oral chemotherapy medications.
Other
medications may cause drowsiness or forgetfulness, interfering with medication
administration conformity.
Even the fear of toxicity may cause some patients to decrease or skip doses
or even take a "drug holiday" to avoid experiencing adverse effects.
Perceptual Barriers
Perceptual barriers that influence oral chemotherapy adherence often result
from inadequate patient
education. Limited
understanding of the drug's dosing regimen, its rationale, benefits, and
adverse effects can also prompt suboptimal adherence. In addition, lack of
written reinforcement about how and when to use each agent, as well as the
medications to manage toxicity, can contribute to perceptual barriers and
problems with optimum adherence.
Patients may have
misconceptions about oral chemotherapy that could interfere with optimal
adherence. One relatively common perception is that oral chemotherapy "is not
as strong" as IV chemotherapy.1 If a patient does not believe
that the balance between benefits and costs favors continued adherence,
regimen completion may be suboptimal. Treatment expectations may be
particularly important with long-term therapies that may have adverse effects
in the short term but have benefits that may be realized only with longer term
use.1
Finally, some health care providers may be misinformed about appropriate
dosing and administration methods of oral chemotherapy used to treat
noncancerous conditions (e.g., methotrexate).1
Physiologic Barriers
While suboptimal adherence affects all age groups, the elderly may exhibit
more problems due to visual and/or cognitive impairment, memory deficits, and
physical limitations.5 Compromise in visual acuity may limit
accurate reading of instructions. Cognitive impairment such as memory deficits
may promote confusion, especially in the context of polypharmacy. An inability
to identify correct medications, open the medication containers, and identify
the proper dose and timing of administration can also pose significant
challenges to patient adherence.4 Because cancer is primarily a
disease of the elderly, these factors may play a particularly important role
in adherence to oral antineoplastic agents. Depression and anxiety, which may
be comorbid conditions or emotional reactions to the intrusion of cancer, can
also affect patient adherence.17 A history of noncompliance is an
important indicator of future behavior and will need to be addressed to attain
optimal patient adherence.
Social Barriers
Numerous social
barriers to adherence have been identified, although more research is needed
to determine their
relative importance. Some of these include:
• The
relationship between patients and their health care practitioners;
• Poor
communication and a lack of trust between clinicians and patients; and
• Language barriers, low
literacy, and cultural and/or religious beliefs about the role of medication
and the ability of an intervention to alter outcomes.
In addition, the role of the family in
patient adherence should not be underestimated. Because family members are
often involved in the daily administration of medications, it is important
that the family understand the dosing schedule, the potential benefits and
adverse effects of the medication, and side effect management along with the
importance of adherence. Individuals that have limited or inadequate support
from family members or friends may have problems carrying through with the
protocol, especially if it is complex and lengthy.
IDENTIFYING NONADHERENCE TO ORAL ANTINEOPLASTIC AGENTS
Although most research indicates
that adherence rates are low, clinicians generally assume that patients take
their medications as prescribed.5 Subjective assessments of
adherence by health care providers are usually unreliable for assessing
medication use.6 Even when clinicians are aware of the possibility
of adherence problems, many health care providers are unable to accurately
predict which patients will adhere to therapy.
However, recognizing indicators and risk
factors for nonadherence can help health care practitioners determine which
patients might be at risk for suboptimal adherence. Key predictors of
adherence problems
are listed in TABLE 2.3 When these factors are present,
health care practitioners should be aware of the possibility of adherence
deterrents, but nonadherence can also occur in the absence of these
indicators. Consequently, suboptimal adherence should always be considered
when a patient's condition does not respond to treatment.

Methods for Assessing Adherence
There is no gold standard
measurement for evaluating adherence.6 Both direct and indirect
techniques for evaluation have been used, each of which has limitations.
Direct measures of adherence are often
impractical, expensive, and may be influenced by the patients' awareness of
the assessment (i.e., the fact that patients are being studied may affect
adherence).6 These measures of adherence include on-site dose
consumption
observation and blood assay measurement.
Indirect measures include pill counts, questionnaires, self-reports,
electronic monitors, refill rates, and pharmacy record reviews. Pill counts
can be unreliable because they can be manipulated and do not indicate
adherence to a particular dosing schedule. Memory-enhancing devices in the
form of computerized dispensing machines, containers separating doses by
schedule requirement, diaries to document medication use, watches sending
signals to take medications, and even services to call patients to prompt
medication taking, while beneficial, still do not ensure that the patient will
take the medication as prescribed. Patient self-reports have also been
criticized as being inaccurate owing to their subjectivity. However, asking
patients in a nonjudgmental manner how often they miss doses may make patients
more comfortable disclosing problems and help health care providers identify
and address adherence deterrents
.
The microelectronic monitoring system (MEMS) is a relatively new method that
uses a tablet bottle that records the date and time the cap is removed.5
Data are collected, recorded, and processed to analyze the number of doses
taken, the number of missed doses, and the dosing intervals.6
However, the MEMS has its limitations. Even if a patient opens the bottle, it
does not guarantee that he or she took the pill as prescribed. Nonetheless, it
may help provide a more accurate assessment of a patient's degree of
adherence.
Pharmacy and insurance records
are often useful tools for evaluating adherence in large populations during
long periods of time.6 This method likely provides the most
accurate estimate of actual medication use in a large number of patients.
However, the utility of the method may be limited by the specificity of the
population included, which may make the data difficult to generalize to other
populations and the investigator unable to determine reasons for treatment
discontinuation.
ENHANCING ADHERENCE WITH ORAL CHEMOTHERAPEUTICS
Use a Multidisciplinary Approach
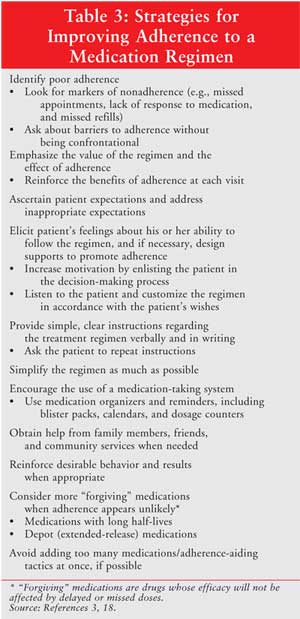
Interventions that include
pharmacists, nurses, and behavioral specialists, in addition to physicians,
have been shown to improve adherence.3 Therefore, all health care
professionals who care for patients using oral antineoplastic agents should be
made aware of adherence issues and should reinforce the importance of
adherence to these medications to patients.2
Another key strategy for
improving patient adherence is to enhance communication between all members of
the health care team and patients.3 Regularly scheduled team
meetings to evaluate patient responses to treatment regimens are helpful in
the collaborative determination of issues and potential impediments to optimum
therapeutic outcomes. Health care providers should develop a rapport with
patients receiving oral chemotherapies and their caregivers to help them feel
comfortable enough to ask questions about their treatment, and perhaps more
important, to be honest about how often they do not adhere to their prescribed
regimens.
Provide Comprehensive
Patient/Family Education
The complexity of cancer
treatment regimens and risk variables specific to the patient population
dictate the type and degree of education about prescribed treatments. Patients
should understand the treatment regimen's potential benefits and adverse
effects. Patient education should address the appropriate use of medications
and provide information about the dose, frequency and timing of dosing, what
to do if a dose is missed, and what to do if adverse effects occur. Directions
should be made clear, kept simple, and provided in writing. Health care
providers should also explain the importance of patient adherence, including
the possible effects of nonadherence. In addition, patients should be advised
to avoid altering treatment on their own. All of these interventions should be
ongoing, rather than a one-time intervention at the initiation of therapy.
Health care professionals should confirm
that patients understand the information they received by asking patients to
repeat dosing instructions and discussing the patients' expectations for
treatment. Involving the patient in the decision-making process about
treatment may also increase patient motivation and enhance adherence.
Because primary caregivers and
extended family can influence a patient's adherence significantly, and in some
cases, may administer the therapies, involving them in the educational process
may facilitate adherence.5 Because of the complexity of
chemotherapy, educating additional caregivers is beneficial even when the
patient is capable of following the treatment regimen without assistance.
Simplify Treatment Regimens
The use of complex chemotherapeutic regimens is a key risk factor for patient
nonadherence. Therefore, simplifying treatment regimens is likely to improve
adherence. Pharmacists can advise clinicians on ways to simplify treatment
regimens and individualize interventions according to the patient's lifestyle
and needs. For example, using an extended-release or a long-acting formulation
instead of an immediate-release formulation may reduce the number of daily
doses and enhance the convenience of treatment. It is especially important to
consider the timing of medication use to determine the most appropriate and
convenient dosing strategy for a particular patient. This is especially
indicated in older cancer patients where polypharmacy is often the norm.
In addition, using packaging
and bottling that is easy to open and read may enhance treatment acceptance
for elderly patients with impaired vision and limited manual dexterity.
Provide Consistent Follow-up
Consistent follow-up is critical
to optimal patient adherence. At each visit, health care providers should
inquire about and monitor the patient's adherence and persistence with
therapy. They also should provide regular counseling and education about the
potential benefits of treatment and risks of poor adherence.
Use Strategies to Improve
Memory
Patients frequently cite
forgetfulness as the most common reason for not taking medication.3
Therefore, interventions that improve memory are likely to enhance patient
adherence. Several cost-effective strategies are available that may help
patients remember to take their medication. Patients should be encouraged to
develop a home dosing routine for their medication use--a routine that enables
a patient to take their medication at the same time each day and that involves
cues that prompt medication-taking rituals and enhance memory.
Health care practitioners should
encourage the use of medication adherence aids, such as calendars, pillboxes
with built-in timer alarms, dosage counters, multi-alarm wrist watches, pagers
with alarm and text reminders, medication diaries, phone reminders,
computerized medication schedulers, and other adherence tools.5
Individualized strategies that combine verbal reminders, written reminders,
and technology may be most effective.
Evaluating Interventions to Improve Adherence
While not comprehensively
investigated, preliminary evidence suggests that interventions designed to
increase adherence are successful in patients using oral chemotherapy. For
example, in one study evaluating adherence to allopurinol and prednisone in
patients with hematologic malignancies, complete adherence with the regimen
occurred in only 17% of patients.10 However, when measures designed
to facilitate adherence were used, such as patient education, home
psychological support, and exercises in pill taking, adherence increased
nearly threefold. Additional research is needed to determine the impact of
strategies to improve adherence with oral antineoplastic therapies and patient
outcomes.
THE ROLE OF THE PHARMACIST
Pharmacists play an important role in determiningadherence and offering advice
about simplifying and improving antineoplastic drug regimens.17
Pharmacists may play a particularly critical role in improving patient
adherence because of their specialized training and expertise in drug therapy,
knowledge of drug–drug and drug–food interactions, access to patient
prescription profiles, practical knowledge about organizing drug treatment
plans, access to patients, and approachability. By establishing trust with
patients, providing support and education, implementing appropriate treatment
plans, and providing effective follow-up, pharmacists have the potential to
significantly improve adherence and outcomes in patients using oral
chemotherapy agents.
Impact of
Pharmacists and Interventions to Improve Adherence
Although the impact of pharmacists on patient adherence to oral antineoplastic
therapy has not been evaluated, several recent studies have demonstrated that
pharmacists can significantly improve adherence to other types of treatment
regimens.19-21 The first study, the Federal Study of Adherence to
Medications in the Elderly, was a multiphase, single-center study of the
efficacy of a comprehensive pharmacy care program in community-based patients
ages 65 and older taking at least four chronic medications.19 The
pharmacy care intervention included patient education, regular follow-up by
pharmacists, and medications dispensed in time-specific compliance packs.
After all patients had participated in a six-month intervention period,
subjects were randomized to the continued pharmacy care program or usual care
for an additional six months. Outcome assessments included change from
baseline in the percentage of pills taken, blood pressure (BP), and
low-density lipoprotein cholesterol (LDL-C) levels.
At baseline, medication adherence
was 61.2%. After 6 months of the intervention, medication adherence increased
to 96.9% and patients experienced significant improvements in hypertension and
LDL-C. Six months after randomization, persistence of medication adherence was
sustained at 95.5% in the pharmacy care group and dropped to 69.1% among
patients assigned to usual care. Significant reductions in systolic BP were
observed in the pharmacy care group but not in the usual care group. Thus, the
pharmacy care program increased medication adherence and persistence and
provided clinically meaningful reductions in BP, whereas discontinuation of
the program was associated with decreased adherence.
The impact of a brief
intervention designed to improve adherence to treatment regimens was also
evaluated in the Diabetes Prevention Program, a randomized, controlled study
evaluating the impact of several interventions on the development of diabetes.
20 At each visit, case managers promoted adherence using a brief
structured interview in which patients were asked about strategies that helped
them take their medications, barriers to adherence that they had encountered,
and strategies that might help them deal with these barriers. The most
frequently reported barrier to adherence was forgetfulness, reported by 22% of
patients. Odds of nonadherence increased with the number of reported barriers,
while odds of adherence increased with the number of strategies used to take
medication. Patients with 80% or greater adherence had a significantly lower
likelihood of developing diabetes. Their finding that increased adherence was
associated with a reduced risk for diabetes supports the use of brief
interventions to address poor adherence in clinical settings.
Another recent study
evaluated the impact of pharmacist interventions in low-income patients with
heart failure.21 In this study, the pharmacist intervention was a
nine-month multilevel program that included a baseline interview, verbal and
written patient educational materials designed for patients with low health
literacy, monitoring of medication use, and communication to clinic nurses and
primary care practitioners. Pharmacists were trained on guidelines for
treating heart failure, key concepts in the pharmaceutical care of older
adults, communication techniques, and the pharmacotherapy of cardiovascular
drugs for heart failure. Patients who received usual care received
prescription services from rotating pharmacists who did not receive additional
specialized training. The usual care group also did not receive the
patient-centered educational materials that were distributed to the group
receiving the pharmacist intervention. Patients in both groups were then
observed in a three-month poststudy phase.
After nine months,
medication adherence was 78.8% in the intervention group and 67.9% in the
usual care group. The rate of emergency department visits and hospital
admissions was 19.4% lower with pharmacist care, as were annual direct health
care costs. However, the difference in treatment adherence dissipated in the
postintervention follow-up period. Adherence rates were only 70.6% in the
intervention group and 66.7% in the usual care group three months after the
intervention ended. The authors concluded that a pharmacist intervention can
improve adherence and decrease health care use and costs, but ongoing
intervention may be required because the benefit appears to diminish once the
intervention ceased.
CONCLUSIONS
Inadequate
patient adherence to medications is highly
prevalent in clinical practice focusing on chronic illness. Until recently,
nonadherence to oral cancer therapies was deemed a relatively small problem
because most medications were delivered intravenously. With the advent of
greater numbers of oral antineoplastic agents, active against a range of
primary tumors,
nonadherence is likely to become an increasingly significant problem.
Owing to pharmacists'
pharmacologic expertise, access to patients, and practical knowledge, they can
play an important role in providing patient education, monitoring patients,
and addressing adherence issues. An understanding of potential barriers,
enhancement strategies, and patient populations at high risk for nonadherence,
as well as the importance of regular patient follow-up, can help pharmacists
address adherence issues and make a significant difference in outcomes from
novel cancer therapies. New techniques for individualizing patient care and
improving adherence, as well as additional research in patient adherence to
oral cancer therapy, is needed to optimize outcomes in these patient
populations.
References
1. Bedell CH. A changing paradigm for cancer treatment: The advent of new oral chemotherapy agents. Clin J Oncol Nurs. 2003;7 supplement(6):5-9.
2. Blasdel C, Bubalo J. Adherence to oral cancer therapies: meeting the challenge of new patient care needs. Oncology Special Edition (Annual Special Report from the publisher of Clinical Oncology News, 2006), conference edition.
3. Osterberg L, Blaschke T.
Adherence to medication.
N Engl J Med.
2005;353(5):487-497.
4. Goldberg RM, Rothenberg ML, Van CE, et al. The continuum of care: a paradigm for the management of metastatic colorectal cancer. Oncologist. 2007;12(1):38-50.
5. Hartigan K. Patient education: the cornerstone of successful oral chemotherapy treatment. Clin J Oncol Nurs . 2003;7(6 Suppl):21-24.
6. Partridge AH, Avorn J, Wang PS, et al. Adherence to therapy with oral antineoplastic agents. J Natl Cancer Inst. 2002;94(9):652-661.
7. Escalada P, Griffiths P. Do people with cancer comply with oral chemotherapy treatments? Br J Community Nurs. 2006;11(12):532-536.
8. Lebovits AH, Strain JJ, Schleifer SJ, et al. Patient noncompliance with self-administered chemotherapy. Cancer . 1990;65(1):17-22.
9. Nilsson JL, Andersson K, Bergkvist A, et al. Refill adherence to repeat prescriptions of cancer drugs to ambulatory patients. Eur J Cancer Care (Engl). 2006;15(3):235-237.
10. Levine AM, Richardson JL, Marks G, et al. Compliance with oral drug therapy in patients with hematologic malignancy. J Clin Oncol. 1987;5(9):1469-1476.
11. Tsang J, Rudychev I, Pescatore SL. Prescription compliance and persistency in chronic myelogenous leukemia (CML) and gastrointestinal stromal tumor (GIST) patients (pts) on imatinib (IM). J Clin Oncol. 2006;24(18S):330s. Abstract.
12. Wood WC, Budman DR, Korzun AH, et al. Dose and dose intensity of adjuvant chemotherapy for stage II, node-positive breast carcinoma. N Engl J Med. 1994;330(18): 1253-1259.
13. Mayer RJ, Davis RB, Schiffer CA, et al. Intensive postremission chemotherapy in adults with acute myeloid leukemia. Cancer and Leukemia Group B. N Engl J Med. 1994;331(14):896-903.
14. Bonadonna G, Valagussa P. Dose-response effect of adjuvant chemotherapy in breast cancer. N Engl J Med . 1981;304(1):10-15.
15. Henk HJ, Thomas SK, Feng W, et al. The impact of non-compliance with imatinib (IM) therapy on health care costs. J Clin Oncol. 2006;24(18S):321s. Abstract.
16. Vermeire E, Hearnshaw H, Van RP, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharmacol. 2001;26(5):331-342.
17. Simpson RJ, Jr. Challenges for improving medication adherence. JAMA. 2006;296(21):2614-2616.
18. Haynes RB, Wang E, Da Mota Gomes M. A critical review of interventions to improve compliance with prescribed medications. Patient Educ Couns. 1987;10:155-166.
19. Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296(21):2563-2571.
20. Walker EA, Molitch M, Kramer MK, et al. Adherence to preventive medications: predictors and outcomes in the Diabetes Prevention Program. Diabetes Care. 2006;29(9):1997-2002.
21. Murray MD, Young J, Hoke S, et
al. Pharmacist intervention to improve medication adherence in heart failure:
a randomized trial. Ann Intern Med. 2007;146(10):714-725.
Enhancing Patient Adherence
to Improve Outcomes With Oral Chemotherapy
Proceedings from a Symposium at the 2007 Hematology/Oncology Pharmacy Association Annual Conference.
A continuing education activity
sponsored by the Hematology/Oncology Pharmacy Association
Release date:
October 2007
Expiration date:
October 31, 2008
Estimated time to
complete activity: 90 to 100 minutes
Sponsored by the Hematology/Oncology Pharmacy Association (HOPA)
This activity is supported by an
educational grant from Pfizer.
TARGET AUDIENCE:
This program is intended for hematology/oncology pharmacists.
GOAL:
To provide pharmacists with practical information on improving patient
adherence to oral cancer therapy.
EDUCATIONAL OBJECTIVES:
After completing this article, participants will be able to:
1. Discuss the impact
of poor patient adherence on clinical outcomes.
2. Recognize
characteristics of populations that are likely to be nonadherent to oral
cancer therapies.
3. Describe methods
that can be used to assess and monitor adherence and their strengths and
weaknesses.
4. Identify and
implement practices that can improve patient adherence.
ACCREDITATION STATEMENT:
The Hematology/Oncology Pharmacy Association is accredited by the
Accreditation Council for Pharmacy Education as a provider of continuing
education.
CREDIT DESIGNATON:
The Hematology/Oncology Pharmacy Association designates this continuing
education activity for 1.5 contact hours (0.15 CEUs) of ACPE credit.
(Universal Program Number 465-000-07-015-H01). A statement of credit will be
issued only upon completion of the post-activity evaluation form and post-test
exam, with a passing grade of 70% achieved.
Individuals who attended the
Enhancing Patient Compliance to Improve Outcomes With Oral Chemotherapy
lecture, presented at HOPA 2007 on June 14, 2007, and claimed live CE credit,
are ineligible to claim credit for completing this monograph.
DISCLOSURE OF CONFLICTS OF
INTEREST: HOPA assesses
conflict of interest with its instructors, planners, managers, and other
individuals who are in a position to control the content of CE activities. All
relevant conflicts of interest that are indentified are thoroughly vetted by
HOPA for fair balance, scientific objectivity of studies utilized in this
activity, and patient care recommendations. HOPA is committed to providing its
learners with high quality CE activities and related materials that promote
improvements of quality in health care and not a specific proprietary business
interest of a commercial interest.
Reported Areas of
Conflict: Faculty
Ms. Boyle has
no actual or potential conflict of interest in relation to this program.
Dr. Bubalo has received
fees for non-CME services from Merck and Pfizer and has been contracted for
research by Merck, Ortho Biotech, and Cubist.
Reported Areas of
Conflict: Planners and Managers
Maryjo Dixon,
RPh, MBA: No significant financial relationships to products or devices.
Charlene Powell, ELS:
No significant financial relationships to products or devices.
Nicole Cooper: No
significant financial relationships to products or devices.
U.S. Pharmacist
does not view the existence of relationships as an implication of bias or
that the value of the material is decreased. The content of the activity was
planned to be balanced, objective, and scientifically rigorous. Occasionally,
authors may express opinions that represent their own viewpoint. Conclusions
drawn by participants should be derived from objective analysis of scientific
data.
METHOD OF PARTICIPATION:
There are no fees for participating and receiving CE credit for this activity.
During the period of October 1, 2007 through October 31, 2008, participants
must 1) read the learning objectives and faculty disclosures; 2) study the
educational activity; 3) complete the online post-test by recording the best
answer to each question from the choices provided; and 4) complete the
online evaluation form. A statement of credit will be issued only upon
submission of a completed activity evaluation form and post-test exam with a
score of 70% or better.
HOW TO ACCESS ONLINE
POST-TEST AND POST-ACTIVITY EVALUATION FORM:
The post-test exam and post-activity evaluation form are available at
cmeuniversity.com. Click on the left-frame link labeled, "Find Post-Tests by
Course" and enter the Course ID 5068 in the Course ID box. You can also locate
the post-test by typing in Adherence" on the same page next to the box labeled
"Search by Part of the Course Title." You will arrive at a page that requires
you to create a user profile. The information you provide will be used to
generate your CE certificate. Once this information is submitted, you will be
taken to the actual evaluation form and post-test exam.
Upon passing the exam with a score
of 70% or better, you will be able to print out your statement of credit
immediately. You can also view your certificate and statement activity and
print out a duplicate statement at any time by visiting cmeuniversity.com.
DISCLOSURE OF UNLABELED USE:
This educational activity may contain a discussion of published and/or
investigational uses of agents that are not indicated by the FDA. HOPA and
Pfizer do not recommend the use of any agent outside of the labeled
indications. The opinions expressed in the educational activity are those of
the faculty and do not necessarily represent the views of HOPA or Pfizer.
Please refer to the official prescribing information for each product for a
discussion of approved indications, contraindications, and warnings.
DISCLAIMER:
Participants have an implied responsibility to use the newly acquired
information to enhance patient outcomes and their own professional
development. The information presented in this activity is not meant to serve
as a guideline for patient management. Any procedures, medications, or other
courses of diagnosis or treatment discussed or suggested in this activity
should not be used by clinicians without evaluation of their patients'
conditions and possible contraindications or dangers in use, review of any
applicable manufacturer's product information, and comparison with
recommendations of other authorities.
The post-test exam and post-activity evaluation form are available at www.cmeuniversity.com.
Exam Questions
1. Which of the
following is an accurate definition of adherence to medication?
A. The extent
to which patients take their medications as prescribed by their clinicians
B. Patients'
willingness to follow a prescribed course of treatment
C. The disposition or
tendency of patients to yield to the will of their clinician
D. The rate at
which patients comply with the medication regimen that their clinicians demand
2. Why is adherence to
cancer therapies an increasingly important issue in cancer care?
A. The use of
oral cancer therapies is increasing
B. Oral cancer
therapies can be administered in less controlled settings than IV therapies
C. Patients
receiving oral agents may receive less education and have less contact with
health care professionals than patients receiving IV medications
D. All of the above
3. Which of the following is
not an advantage of oral cancer therapies compared to IV therapies?
A. Greater
convenience
B. Less time away
from work and family
C. Greater
monitoring and supervision required by health care professionals
D. Potential for
attenuated adverse effects compared to traditional therapy
4. Which of the following
statements best describes adherence rates with oral cancer therapies?
A. Adherence
to oral cancer therapies is higher than adherence to other therapies because
of the gravity of cancer
B. Rates of
adherence to long-term medications that reduce mortality are higher than those
observed with other long-term medications
C. Adherence to oral
cancer therapies is not necessarily higher than that observed with other
long-term therapies
D. Adherence to
oral cancer therapies is lower than that seen with other long-term therapies
5. What is a potential
outcome of poor adherence to oral cancer therapies?
A. Inferior
disease-free survival
B. Higher rates of
hospitalization and longer hospitalizations
C. Unnecessary
changes in drug regimens and unnecessary diagnostic testing
D. All of the above
6. Overadherence, a type of
nonadherence that may occur in patients using oral cancer therapies:
A. Is
characterized by a fear that oral agents may not be sufficiently effective,
causing patients to overuse the agent(s)
B. Does not occur
in patients with other disease states
C. Does not affect
the risk of drug toxicity
D. Improves
outcomes
7. Which of the following best
describes the key determinant of a patient's adherence to long-term
interventions?
A. Actual
risks, benefits, and costs of the intervention
B. Patient's
perception of the risks, benefits, and costs of the intervention
C. Types of
barriers to adherence that the patient experiences
D. Patient's need
for the intervention
8. Which of the following
is a logistical barrier to patient adherence to oral cancer therapies?
A. Treatment
complexity and/or high dosing frequency
B. Cost of
treatment
C. Polypharmacy
D. All of the above
9. Which of the following
is a perceived barrier to adherence that may be unique to oral cancer
therapies?
A. A poor
understanding of the dosing regimen
B. Fear of the
adverse effects of oral cancer therapies
C. The belief that
oral cancer therapies are "not as strong" as IV therapies
D. Visual or
cognitive impairment in the elderly
10. Which of the following
is not a barrier to treatment adherence?
A. Low literacy
B. Effective
support of the treatment by the patient's family and/or caregiver
C. Lack of trust
between clinicians and patients
D. Inadequate
understanding about the ability of a treatment to affect outcomes
11. Which of the following
is a predictor of poor patient adherence to medication?
A. Presence of
psychological problems, particularly depression
B. Inadequate
follow-up
C. Patient's lack
of insight into the illness
D. All of the above
12. Which measurement for
evaluating adherence is the gold standard assessment method in clinical
practice?
A. There is no
gold standard method
B. The
microelectronic monitoring system
C. Blood assays or
physiologic markers of the agent
D. Pill counts
13. Which of the following
assessments provides the most accurate estimate of actual medication use in a
large number of patients?
A. The
microelectronic monitoring system
B. Clinical
responses
C. Reviews of
pharmacy and insurance records
D. Patient
self-reports
14. Successful methods of
improving adherence involve each of the following strategies except:
A. Patient
education
B. Addition of
other agents
C. Adequate
patient follow-up
D. Medication adherence
aids
15. In surveys, what is the
most common reason patients cite for not taking their medication?
A. Forgetfulness
B. Cost of therapy
C. Adverse effects
of therapy
D. Poor understanding
of dosing regimen
16. In one study of
adherence in patients with hematologic malignancies using oral cancer
therapies, patient education, home support, and exercises in pill taking
increased adherence rates by _____?
A. Half
B. Twofold
C. Threefold
D. Fourfold
17. Pharmacists can play an
important role in increasing patient adherence because of their:
A. Specialized
training and expertise in drug therapy
B. Practical
knowledge about organizing treatment plans
C. Access to
patients
D. All of the above
18. Pharmacists may be able to
improve rates of patient adherence to oral cancer regimens by:
A. Providing
patient support and education
B. Offering advice
to physicians about simplifying and improving drug regimens
C. Providing
effective follow-up
D. All of the above
19. Which of the following
findings was notreported in a recent study of a pharmacist intervention
in patients on multiple chronic medications?
A. Improvement
in adherence rates
B. Sustained
improvement even after discontinuation of the pharmacist intervention
C. Improvement in
clinical outcomes (e.g., hypertension)
D. Rates of
medication adherence >95%
20. In a study of
low-income patients with heart failure, a pharmacist intervention was
associated with:
A. Reduced
emergency department visits and hospitalizations
B. Sustained
improvement in adherence, even after discontinuation of the intervention
C. Similar rates
of adherence compared to rates seen in the usual care group
D. Increased
health care costs





