US Pharm. 2008;33(11):24-28.
On a regular basis, most pharmacists must interact with patients who have mental illnesses. Accessible settings allow community pharmacists to provide care for these patients. In order to do this effectively, community pharmacists must be sufficiently trained in mental health, as well as be comfortable with these patient interactions. Background information on mental illness, plus tips on how to counsel patients with depression, is provided, with the intent to enhance the professional relationship between community pharmacists and patients with depression.
Prevalence
Mental illness occurs in approximately 26.2% adults in America.1 Depression, one of the most prevalent mental illnesses, affects about 14.8 million adults in the United States every year.2 Major depressive disorder is the leading cause of disability for Americans between the ages of 15 and 44.2 Furthermore, it has been estimated that by the year 2030, depression will be one of the top three leading causes of burden of disease.3 Pharmacists have an opportunity to make a positive impact on this patient population and the outcome of treatment. However, first we must overcome the ever-present stigma associated with mental illness and its treatment.
Impact of Stigma
Patients who receive psychotropic medications are often stigmatized. In one study, 28% of mental health care consumers surveyed reported being stigmatized by mental health caregivers.4 Of these consumers, 95% reported experiencing long-term consequences subsequent to stigmatization endured from family, friends, and coworkers. Consequences included lower self-esteem and self-confidence, fewer disclosures surrounding their illness, and increased isolation. Such consequences can have a negative impact on the patient-pharmacist relationship, yet they can be overcome. One study evaluated the effectiveness of telemonitoring as a tool to enhance education and monitoring in order to improve communication between patients and pharmacists.5 Specifically, pharmacists were able to identify misperceptions, patient concerns, and treatment progress. Health care providers must be cognizant of their own attitudes regarding mental illness, the effect stigma has on their patients, and how it will impact the pharmacist–patient relationship.
A study by Phokeo et al reported on the impact stigma may have in the community pharmacy setting.6 The authors surveyed community pharmacists to evaluate pharmacists' attitudes toward patients receiving psychotropic and cardiovascular medications. Pharmacists reported feeling more uncomfortable discussing symptoms of mental illness and drug indication with patients receiving psychotropic medications. They also felt that patients with mental illness were less likely to discuss their symptoms and to require less monitoring compared to patients treated with cardiovascular medications. However, pharmacists did acknowledge that patients with mental illness are less likely to obtain pharmacy services and were in need of drug information. Educating community pharmacists about the symptoms of mental illness, as well as the importance of monitoring and patient interaction on this level, may lead to increased utilization of pharmacy services, which could greatly benefit this patient population.
A survey of pharmacists in Alabama also reported on the attitudes toward providing care to patients with mental illness.7 As with Phokeo et al, pharmacists had positive attitudes toward this patient population. However, when asked about confidence, comfort level, and interest in providing medication counseling, over half of the respondents were neutral or less likely to provide these services if the patient was mentally versus physically ill. Generally, pharmacists have positive attitudes toward patients with mental illness and recognize the importance of providing quality patient-centered care. Nonetheless, certain barriers must be addressed in order to improve patient–pharmacist interactions.
Barriers to Counseling
Barriers in providing medication counseling to patients with mental illness are numerous. These include a lack of privacy, impaired ability to communicate based on patient symptoms, lack of time, lack of patient-specific information, and inadequate training.6 Additionally, counseling patients on psychotropic medication poses its own risks and challenges. Along with drug information, pharmacists should address adherence.8 Furthermore, patients have their own misconceptions about psychotropic medications. Americans report that psychotropic medications are effective, yet most are unwilling to take them, with 23.3% of respondents believing they are harmful to the body.9 This unwillingness increases the difficulties pharmacists may encounter when counseling patients.
Community Pharmacists' Impact on Depression
Despite these barriers, community pharmacists can have a large impact on the care of patients with depression. In a study involving rural community pharmacies, the intervention pharmacists were provided with training to enhance their advice and support for patients with depression, while control pharmacists provided usual care.10 While well-being was notably improved in both groups, intervention-group patient attitudes about drugs, as well as medication adherence, were improved. This study indicates that pharmacists can have a positive impact, regardless of level of training.
Patient Response to Counseling
Patients are commonly in search of more information regarding their disease state and treatment. In a recent study, patients newly diagnosed with depression were evaluated for preference of education by a pharmacist.11 Pharmacist interventions consisted of either a written patient leaflet or an intensive 10-minute, drug-related counseling session. Forty-nine percent of patients reported that their medication concerns were answered by their physician; however, 90.4% favored receiving further information. Some patients even reported that pharmacist-intense counseling was more comprehensive than the provider's explanation. Pharmacists can serve as an additional resource and should provide thorough counseling on antidepressant medication.
Counseling: Are Pharmacists Doing Enough?
In 1993, the Omnibus Budget Reconciliation Act of 1990 (OBRA 90) went into effect, requiring pharmacists to counsel every Medicaid patient.12 Individual states were given the opportunity to adopt additional requirements, and 90% of the states adopted OBRA 90 regulations for all patients.13 Fifteen years later, patient counseling remains inconsistent. Svarstad et al described counseling practices at pharmacies via a trained patient with a new prescription for amoxicillin, ibuprofen, or paroxetine.14 Twenty-five percent of pharmacists never spoke to the patient. Overall, 59% of patients with a prescription for paroxetine received some degree of verbal information. However, only 22.9% of patients were told about duration of treatment, only 36.6% received adverse effect information, and only 15.7% were told when paroxetine would begin to work. Given the narrow scope of counseling that was reported, it is not surprising that nearly 30% of patients receiving an initial antidepressant discontinue treatment during the first month.15 Community pharmacists should understand the influence they can have on the treatment of depression and should individualize counseling strategies to optimize care.
Another study examined drug coaching by community pharmacists and its effect on patient attitudes toward drug therapy.16 The survey utilized found that 77% of patients in the intervention group (versus 57% in usual care) disagreed with the statement, "I don't need to take medications once I feel better." Furthermore, 86% of the intervention group found contact with a pharmacist helpful in taking an antidepressant versus 52% in the control group. When patients receive more initial counseling, especially in terms of side effects, time to effect, and methods for follow-up, they are better informed and equipped to handle the outcomes of treatment. Thus, a trusting pharmacy relationship is established, which should foster adherence and follow-up.
Model for Counseling
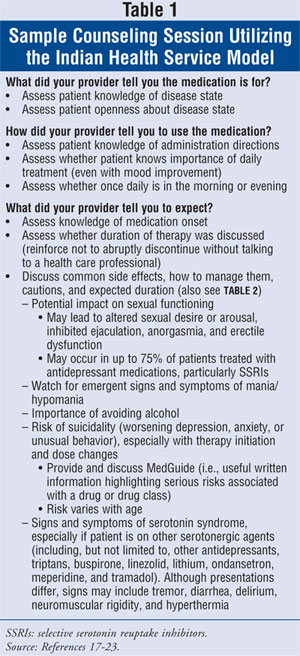
Many pharmacists are trained to counsel using the Indian Health Service (IHS) Model. While not all-inclusive, TABLE 1 shows an example of how a counseling session may be framed utilizing the IHS model.17-23 Additionally, various counseling tips are provided regarding antidepressant medications. Possible adverse effects are discussed in TABLE 2 in further detail.24-29
Given the barriers to counseling and the stigma associated with depression, it is imperative that pharmacies have a private area for a detailed consultation. Counseling sessions should also include refill and missed dose procedures. If a woman is pregnant or breastfeeding, a discussion of risks and benefits should be included. The patient should be given a drug information leaflet and a medication guide with an explanation of their purpose and utility. Lastly, the session should conclude with verification of patient understanding and an offer of availability along with contact information for follow-up.
Motivational Interviewing
In addition to more comprehensive counseling, pharmacists can play an important role in the treatment of depression through follow-up and adherence assessment. Adherence involves a partnership between the patient and provider with regard to health-related decisions.30 Pharmacists can utilize many tools to assess and foster adherence, one of which is motivational interviewing (MI). This is defined as a "method for enhancing intrinsic motivation to change by exploring and resolving ambivalence."31 MI utilizes empathic listening and reflective responses to decrease patient resistance and foster conversation about change.32 Pharmacists may incorporate MI into follow-up dialogue with patients to assess adherence and satisfaction with drug therapy.
One study examined outcomes of pharmacist interactions with patients having depression over a six-month period.33 Initial encounters with patients occurred in person (45 minutes) or via telephone or e-mail (13 minutes). Pharmacists' interventions included educating patients in response to questions or misconceptions and utilizing elements of MI to promote adherence. Once a trusting relationship was formed, patients honestly discussed medication-administration habits and disclosed key information in regard to side effects and nonadherence. More important, these habits and concerns were not revealed to the patients'primary care providers. Unfortunately, a busy community pharmacy may not be the best platform to provide 45-minute consultations. On the other hand, community pharmacists offer accessibility and the ability to develop a trusting relationship, and they possess the training to provide patients with information and support. More research needs to examine MI as part of a daily follow-up routine by community pharmacists to optimize care in patients diagnosed with depression.

Conclusion
Despite the barriers discussed, patients with serious and persistent mental illnesses continue to seek reliable information from pharmacists.34 We as pharmacists must be prepared and willing to offer our expertise to patients with depression and other mental illnesses. Furthermore, we need to establish a trusting and supportive relationship with our patients. The initial consultation with a patient presenting a new prescription for an antidepressant is an opportunity to establish this relationship. Pharmacies should have adequate private counseling areas to offer more in-depth information. Pharmacists can also play a key role in assessing and preserving adherence. An effort should be made in the critical first three weeks after a new prescription is filled to follow up with the patient on efficacy and treatment concerns. Being advocates for our patients with depression is just one more example of the type of care community pharmacists are able to provide.
REFERENCES
1. National Institute of Mental Health. Statistics. www.nimh.nih.gov/health/statistics/index.shtml. Updated April 3, 2008. Accessed May 13, 2008.
2. National Institute of Mental Health. The numbers count: mental disorders in America. www.nimh.nih.gov/health/publications/the-numbers-count-mental-disorders-in-america.shtml. Updated May 13, 2008. Accessed May 13, 2008.
3. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:2011-2030.
4. Wahl OF. Mental health consumers' experience of stigma. Schizophr Bull. 1999;25:467-478.
5. Rickles NM, Svarstad BL, Statz-Paynter JL, et al. Improving patient feedback about and outcomes with antidepressant treatment: a study in eight community pharmacies. J Am Pharm Assoc. 2006;46:25-32.
6. Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55:1434-1436.
7. Cates ME, Burton AR, Woolley TW. Attitudes of pharmacists toward mental illness and providing pharmaceutical care to the mentally ill. Ann Pharmacother. 2005;39:1450-1455.
8. Tanskanen P, Airaksinen M, Tanskanen A, Enlund H. Counseling patients on psychotropic medication: physicians' opinions on the role of community pharmacists. Pharm World Sci. 2000;22:59-61.
9. Croghan TW, Tomlin M, Pescosolido B, et al. American attitudes toward and willingness to use psychiatric medications. J Nerv Ment Dis. 2003;191:166-174.
10. Crockett J, Taylor S, Grabham A, Stanford P. Patient outcomes following an intervention involving community pharmacists in the management of depression. Aust J Rural Health. 2006;14:263-269.
11. Al-Saffar N, Abdulkareem A, Abdulhakeem A, et al. Depressed patients' preferences for education about medications by pharmacists in Kuwait. Patient Educ Couns. 2008;72:94-101.
12. OBRA 1990 Regulations. Fed Regist. 1992;57:4937-4940.
13. Sec. XXIII--patient counseling requirements. In: Survey of Pharmacy Law [CD-ROM]. Mount Prospect, IL: National Association of Boards of Pharmacy; 2007:75-76.
14. Svarstad BL, Bultman DC, Mount JK. Patient counseling provided in community pharmacies: effects of state regulation, pharmacist age, and busyness. J Am Pharm Assoc. 2004;44:22-29.
15. Simon GE, VonKorff M, Wagner EH, Barlow W. Patterns of antidepressant use in community practice. Gen Hosp Psychiatry. 1993;15:399-408.
16. Brook O, van Hout H, Nieuwenhuyse H, Heerdink E. Impact of coaching by community pharmacists on drug attitude of depressive primary care patients and acceptability to patients; a randomized controlled trial. Euro Neuropsycho pharmacol. 2003;13:1-9.
17. Lewis RK, Lasack NL, Lambert BL, Connor SE. Patient counseling--a focus on maintenance therapy. Am J Health Syst Pharm. 1997;54:2084-2098.
18. Pfizer, Inc. Pharmacist–Patient Consultation Program--Unit I: An Interactive Approach to Verify Patient Understanding. New York, NY: National Health Care Operations; 1991.
19. Pfizer, Inc. Pharmacist–Patient Consultation Program--Unit II: How to Counsel Patients in Challenging Situations. New York, NY: National Health Care Operations; 1993.
20. Pfizer, Inc. Pharmacist–Patient Consultation Program--Unit III: Counseling to Enhance Compliance. New York, NY: National Health Care Operations; 1995.
21. Taylor MJ, Rudkin L, Hawton K. Strategies for managing antidepressant-induced sexual dysfunction: systematic review of randomised controlled trials. J Affect Disord. 2005;88:241-254.
22. Gregorian RS, Golden KA, Bahce A, et al. Antidepressant-induced sexual dysfunction. Ann Pharmacother. 2002;36:1577-1589.
23. Boyer EW, Shannon M. The serotonin syndrome. N Eng J Med. 2005;352:1112-1120.
24. Kando JC, Wells BG, Hayes PE. Depressive disorders. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York, NY: McGraw-Hill Companies, Inc; 2005.
25. Emsam (selegiline transdermal system) package insert. Princeton, NJ: Bristol-Myers Squibb; February 2008.
26. Holm KJ, Markham A. Mirtazapine: a review of its use in major depression. Drugs. 1999;57:607-631.
27. Micromedex Healthcare Series [Internet database]. Greenwood Village, CO: Thomson Healthcare. Updated periodically.
28. Perry PJ, Alexander B, Liskow BI, DeVane CL. Psychotropic Drug Handbook. 8th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2007.
29. Teter CJ. Counseling patients being treated with antidepressants. Pharmacy Times. February 2004. www.pharmacytimes.com/issues/articles/2004-02_928.asp. Accessed October 7, 2008.
30. Possidente CJ,Bucci KK, McClain WJ. Motivational interviewing: a tool to improve medication adherence? Am J Health Syst Pharm. 2005;62:1311-1314.
31. Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002:22.
32. Scales R, Miller J, Burden R. Why wrestle when you can dance? Optimizing outcomes with motivational interviewing. J Am Pharm Assoc. 2003;43:S46-S47.
33. Bungay KM, Adler DA, Rogers WH, et al. Description of a clinical pharmacist intervention administered to primary care patients with depression. Gen Hosp Psychiatry. 2004;26:210-218.
34. MacHaffie S. Health promotion information: sources and significance for those with serious and persistent mental illness. Arch Psychiatr Nurs. 2002;16:263-274.
To comment on this article, contact
rdavidson@jobson.com






