US Pharm.
2006;31(9):HS-16-HS-24.
According
to the most recent surveillance data from the CDC, hysterectomy is the second
most frequently performed surgical procedure for women of reproductive age,
topped only by cesarean delivery.1 The United States has the
highest rate of hysterectomy in the industrialized world, with 5.5 per 1,000
women undergoing the procedure each year.1,2 Many indications for
hysterectomy are poorly defined and based more on expert opinion than on
evidence from well-designed clinical trials.2,3
Regardless of the surgical
technique used, hysterectomy is associated with short- and long-term
complications. All women considering hysterectomy should be aware of these
risks prior to surgery, in order to make an informed decision as to whether
the procedure is the best treatment option. This article reviews the short-
and long-term complications associated with hysterectomy and thereby aids
pharmacists in providing care for this large population of women.
Indications for Hysterectomy
Health care
providers have limited data from well-designed clinical trials to guide
determination of when hysterectomy is the most appropriate treatment option.
Some well-established indications for hysterectomy include life-threatening
conditions such as serious complications during childbirth, unmanageable
uterine hemorrhage, and invasive cancer of the uterus, cervix, va gina,
fallopian tubes, or ovaries.2,4 Outside of these situations,
however, guidance is scarce regarding the appropriate indications for
hysterectomy.
According to the CDC, from
1994 to 1999, uterine leiomyoma, endometriosis, and uterine prolapse were the
most common indications for hysterectomy and accounted for 73% of all
hysterectomies performed.1 This figure is quite staggering,
considering that much of the current literature recommends conservative
management of most benign gynecologic conditions, with hysterectomy considered
as a last resort in refractory cases.5
In 2002, the Society of
Obstetricians and Gynecologists of Canada (SOGC) published clinical practice
guidelines that provide common indications for hysterectomy.4
According to these guidelines, endometriosis with severe symptoms that are
refractory to other medical treatment options, symptomatic leiomyomas (uterine
fibroids), and pelvic relaxation are benign conditions in which hysterectomy
may be considered. In the case of abnormal uterine bleeding, endometrial
lesions must be excluded and medical alternatives should be considered
first-line therapy prior to consideration of surgical intervention.4
The SOGC guidelines recommend that in all cases pertaining to benign
conditions, risks and benefits of surgery as well as loss of fertility should
be discussed prior to surgery, and a woman's preference should be highly
respected.
Types of Hysterectomy
There are several
types of hysterectomy, all of which include the removal of the uterus. In a
subtotal hysterectomy (also referred to as a supracervical or partial
hysterectomy), the upper two thirds of the uterus is removed, while the cervix
is left in place.2 Although this procedure is common, the majority
of women decide to have a total hysterectomy. A total hysterectomy (or
complete hysterectomy) involves the removal of the entire uterus as well as
the cervix. If both the ovaries and the fallopian tubes are removed during a
total hysterectomy, the procedure is called a bilateral salpingo-oophorectomy.
Finally, the most extreme type of hysterectomy, a radical hysterectomy,
involves removal of the uterus, cervix, ovaries, fallopian tubes and,
possibly, upper portions of the vagina and affected lymph glands. This
procedure is strongly recommended for serious complications and diseases such
as cancer.2
A hysterectomy may be
performed via abdominal, vaginal, or laparoscopic-assisted abdominal or
vaginal approaches.2 The appropriate route of surgery is determined
by the type of pathology expected, anatomic considerations, patient
preference, and physician experience and training. According to the SOGC
clinical practice guidelines, vaginal hysterectomy should be considered the
first choice for all benign indications, while laparoscopic-assisted
approaches should be considered when using such an approach reduces the need
for a laparotomy.4 Although there is limited information concerning
direct comparisons of hysterectomy procedures, preliminary data suggest that
LAVH may be associated with shorter hospital stays, less pain, more rapid
recovery, and fewer complications; however, this approach is associated with
higher surgical costs.1
Surgical and Postsurgical
Complications
Hysterectomy is
generally a safe procedure, but with any major surgery comes the risk of
surgical and postsurgical complications. Such complications commonly include
infection, hemorrhage, vaginal vault prolapse, and injury to the ureter,
bowel, or bladder.6,7 Although hysterectomy is associated with
fewer complications than many other major operations, risks and complications
depend upon the type of hysterectomy performed, the individual woman's health
status, and the surgeon's expertise and experience.4,6,7
Infection:
Postoperative fever and infection are responsible for the majority of minor
complications following hysterectomy. Infection occurs in approximately 6% to
25% of patients who undergo abdominal hysterectomy versus 4% to 10% of those
who undergo vaginal hysterectomy. Despite impeccably sterile surgical
technique and careful patient selection, women undergoing a hysterectomy
procedure have a 30% chance of postoperative febrile infection.2
In both abdominal and vaginal
hysterectomy, pelvic infection occurs in approximately 4% of cases.8,9
Pelvic cellulitis is an infection of the soft tissues and usually occurs
around the third day following surgery. Although some degree of cuff
cellulitis probably occurs following the majority of hysterectomies,
antibiotics are not required unless fever persists. Additionally, the rate of
postoperative symptomatic urinary tract infection is approximately 1% to 5% in
patients who undergo hysterectomy. Immediate catheter removal postoperatively
is strongly recommended to reduce the risk of this complication.8-10
Risk of postoperative
infection can be lowered substantially with the use of prophylactic
antibiotics.8,9 Studies reveal that women who receive prophylactic
antibiotics prior to an abdominal or vaginal hysterectomy have a reduced rate
of wound infection, pelvic cellulitis, vaginal cuff abscess, and pelvic
abscess.9 The proper dosage should be administered 30 minutes prior
to surgery to ensure that therapeutic levels are achieved in tissue at the
surgical site. Agents such as cefazolin, cefotetan, cefoxitin, metronidazole,
and clindamycin have all proved effective.8-10 If postoperative
fever persists and infection is suspected or identified, a broad-spectrum
intravenous antibiotic covering anticipated pathogens should be initiated.
Antibiotics should be continued for 24 to 48 hours after the resolution of
fever and symptoms.8,9
Ureteral Injury:
Ureteral injury is becoming a more frequent posthysterectomy complication as
the number of laparoscopic-assisted procedures increases. The incidence rate
of this complication in laparoscopic-aided procedures is 0.7% to 1.7% with
abdominal hysterectomy and 0% to 0.1% with vaginal hysterectomy.10
Injuries generally occur with excessive electrocautery and lasering adjacent
to the ureter. These injuries are best managed with resection of the damaged
portion and reimplantation of the ureter.11 Surgeons should
recognize urologic injuries and correct them intraoperatively to avoid serious
postoperative complications that occur from urinary extravasation.10,11
Bladder Injury: Injury to the bladder occurs in approximately 0.5% to 2% of all hysterectomies. 8,12 Bladder injury most likely occurs during entry to the peritoneum or during dissection of the bladder off the lower uterine segment, cervix, and upper vagina. Several studies have concluded that partial disruption of the innervation of the bladder during hysterectomy may result in postoperative incontinence.13,14 A systematic review reported that hysterectomy was considered a risk factor for urinary incontinence in women older than 60. 14 In another study, urge incontinence was found to be more common than stress incontinence in women posthysterectomy.13 In 2002, a large cohort study revealed that women older than 50 were less likely to have improvement with urinary incontinence after hysterectomy compared to younger women.15
Bowel Injury:
Although bowel injury is uncommon, particularly with vaginal hysterectomy, it
is a serious complication associated primarily with laparoscopic-assisted
abdominal hysterectomy. During both abdominal and vaginal surgery, the rectum
and ascending and descending colon can be injured.8 Bowel injuries
occur during the lysis of adhesions involving the bowel and dissection of the
posterior cul-de-sac. Preoperative bowel preparations will allow for
incidental colon surgery without the necessity of colostomy. If a large bowel
injury should occur and no preoperative bowel preparation was given, a
temporary diverting colostomy may be indicated to protect the suture line and
lower the risk of peritonitis and sepsis.10
Hemorrhage:
One of the most serious postoperative complications associated with
hysterectomy is hemorrhage. Excessive bleeding complicates approximately 1% to
3% of all hysterectomies.12 In most cases, bleeding originates at
the lateral vaginal angles and is amenable to vaginal resuturing. Average
intraoperative blood loss can range anywhere from 300 to 400 mL.16
Early postoperative signs of hemorrhage after vaginal hysterectomy include
bleeding from the vagina, deterioration in vital signs, decreased hematocrit
level, and flank abdominal pain.
It is routine to cross-match
blood in patients undergoing hysterectomy. Two to four units of packed red
blood cells should be available at all times. Women who are more likely to
need blood transfusion include those undergoing peripartum hysterectomy or
hysterectomy for gynecologic cancer, as well as those undergoing elective
hysterectomy with pelvic inflammatory disease, or pelvic abscesses or
adhesions.10
Thromboembolic Disease:
The risk of venous thromboembolism following abdominal hysterectomy in low-
and high-risk patients is 0.2% and 2.4%, respectively.9,10 The risk
of deep venous thrombosis and pulmonary embolism can be minimized with the use
of graduated compression stockings perioperatively and early ambulation
postoperatively. The type of prophylaxis recommended depends upon each
patient's risk factors. Risk factors include obesity, malignancy, previous
radiation therapy, immobilization, estrogen use, prolonged anesthesia, radical
surgery, and personal or family history of thromboembolic disease. Patients at
high risk for thromboembolism may be given a low-molecular-weight heparin or
5,000 units of subcutaneous heparin preoperatively and then every eight to 12
hours postoperatively to reduce the risk of thromboembolic events.8-10
Fallopian Tube Prolapse:
Fallopian tube prolapse is an uncommon postoperative complication of
hysterectomy. A predisposing factor for prolapse is the presence of a hematoma
or abscess at the vaginal apex.8,9,11 If the tissue does not
respond to conservative treatment, such as cryotherapy or silver nitrate
application, a biopsy of the area may be warranted.9 Surgical
interventions are recommended for the management of fallopian tube prolapse.
8,9
Vaginal Vault Prolapse:
Vaginal vault prolapse is a type of pelvic organ prolapse that can happen
following surgical removal of the uterus. It often occurs when the top of the
vagina loses the support of the uterus and then sags or drops into the vaginal
canal. Most women with vaginal vault prolapse will also have bulging of the
small bowel into the vagina, as well as other bladder and bowel problems such
as urinary incontinence and constipation.6,7,15,16 It is important
to note that vaginal vault prolapse may be treated with a vaginal pessary, a
special device that holds the vagina in place; in some cases, surgery may be
warranted.16
Vaginal Cuff
Evisceration: A rare
complication that can occur following a hysterectomy is evisceration of the
small intestine into the vagina.7,9,17 It is associated with the
Valsalva's maneuver, severe vomiting, or coughing. Symptoms usually include
vaginal bleeding or discharge, abdominal-pelvic pain, pressure in the vagina,
and protrusion of bowel. Although eviscerations usually occur early in the
postoperative period, one study of 12 patients reported occurrence 27 months
after various pelvic procedures.17 Medical treatment usually
includes administration of intravenous fluids and broad-spectrum antibiotics
and immediate laparotomy with replacement of the mesentery and small bowel.
6,7,9
Possible Long-Term
Complications
Many of the
clinical findings concerning the long-term side effects of hysterectomy are
conflicting. Data show some women develop the complication, while others
experience relief from the same complication. For example, some studies have
shown increases in psychosexual dysfunction after hysterectomy, while others
have shown improvements in this area.3,18 Discrepancies in the data
make it difficult for clinicians to clearly identify the long-term risks of
hysterectomy and for women to determine if the possible benefits of
hysterectomy outweigh the risks.
Early Menopause:
Many of the long-term complications associated with hysterectomy arise
secondary to changes in hormonal balance. Bilateral oophorectomy is performed
in more than 50% of hysterectomies in the U.S. and is controversial.1
Some practitioners believe the ovaries should be removed to prevent future
development of malignancy, while others prefer to conserve "normal ovaries" to
preserve sex hormone secretion and avoid long-term hormone therapy (HT),
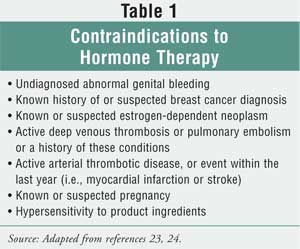
especially in women with contraindications to estrogen therapy (Table 1
).19 When the ovaries are removed, levels of ovarian sex hormones,
namely estrogen, progesterone, and testosterone, rapidly decline, resulting in
sudden menopause.
Studies have found that even
those women who keep one or both ovaries experience menopause at an earlier
age. A retrospective trial found that women who had had a hysterectomy with
preservation of one or both ovaries experienced menopause an average of 5.5
years earlier than women who had not undergone hysterectomy. In this study, no
difference was found between women with one versus both ovaries, though some
studies have reported differences.19 It has been theorized that
early ovarian failure may occur due to disruptions in ovarian blood flow,
which is necessary for proper sex hormone production.19,20
Studies have consistently
shown HT to be effective for the reduction of menopausal symptoms.21-24
Common symptoms of menopause include hot flashes, night sweats, vulvar and
vaginal atrophy, vaginal dryness, insomnia, and sleep disturbances. Initiating
estrogen therapy immediately after hysterectomy with bilateral oophorectomy is
important in order to prevent onset of menopausal symptoms, although some
practitioners may be hesitant to prescribe long-term HT due to the findings
that led to the early termination of the Women's Health Initiative (WHI) trial.
25
In February 2004, the NIH
decided to terminate the WHI estrogen-only trial before its proposed March
2005 end. Because this trial failed to show that estrogen protects women from
coronary heart disease and demonstrated statistically significant increases in
the incidence of stroke and deep venous thrombosis, the NIH deemed it
unacceptable to subject healthy women to these risks and therefore stopped the
trial early. It is important to note that the WHI estrogen-only trial did find
a significant reduction in hip and other fractures, as well as an unexpected
decrease in breast cancer incidence (P = .06). The WHI trial also demonstrated
that when estrogen replacement therapy (ERT) is used for the treatment of
menopausal symptoms after hysterectomy, an overall balance of risks and
benefits exists, and most importantly, no effect on total mortality was seen
throughout the 6.8-year follow-up period.25
Women whose ovaries are
preserved should be counseled concerning common menopausal symptoms, and
estrogen therapy may be considered when these symptoms are present.19
The duration of ERT after hysterectomy has been debated, and no current
guidelines are available to aid practitioners with this treatment decision.
Many clinicians are now using ERT through the average age of natural menopause
(approximately age 50) and then tapering women off therapy slowly to help
prevent reappearance of symptoms.25 If symptoms recur during dose
tapering, ERT may need to be restarted or nonhormonal agents may be tried.
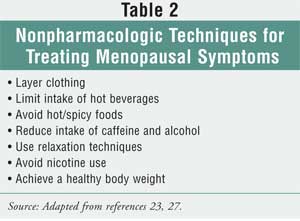
Nonpharmacologic techniques for treating menopausal symptoms are outlined in
Table 2. If a woman simply undergoes oophorectomy and her uterus is
preserved, progesterone should be added to the treatment regimen to prevent
endometrial hyperplasia.24,26
Impaired Sexual Function:
Studies have found
that concern about posthysterectomy sexual dysfunction is the most common
cause of anxiety for women undergoing the procedure.20 There are
many plausible mechanisms by which sexual dysfunction may occur, including
shortening of the vagina, disruption of innervation of the vagina, and vaginal
dryness due to estrogen deficiency.3,20,28,29
Conversely, sexual function
may improve posthysterectomy. It has been postulated that sexual function is
improved through relief of pain during intercourse due to removal of pelvic
pathology, relief of dysmenorrhea, and increased libido due to decreased fear
of conception.20
Clinical data are split
concerning the true effects of hysterectomy on a woman's sexual function.
Early retrospective data found that hysterectomy causes a significant decline
in sexual function.3 To the contrary, more current data derived
from prospective clinical trials show improvements in sexual function,
including increases in frequency of intercourse, sexual desire, and strength
and occurrence of orgasms, as well as reductions in dyspareunia.20,28
It was once thought that
retaining the cervix would result in less sexual dysfunction due to a decrease
in neurologic and anatomic disruption, although clinical trials have not
supported this theory.28,29 A 2003 prospective observational study
examined the differences between the effects of vaginal, subtotal abdominal,
and total abdominal hysterectomy on sexual function and found significant
improvements in sexual function with all three types of hysterectomy, with no
significant differences among the three types.28
Psychological Effects
Data are also mixed concerning the
effects of hysterectomy on psychological functioning. As seen with other
complications of hysterectomy, retrospective studies have reported adverse
psychological outcomes, whereas prospective studies have not supported these
claims.3 In fact, prospective studies have shown that hysterectomy
improves mood and quality of life in many women by relieving preexisting
distressing gynecologic symptoms.3,26
It has been well established
that one of the most important influences on postoperative psychiatric
morbidity is preoperative psychiatric state.26 Women with
psychiatric illness prior to surgery are much less likely to show improvement
in this regard after hysterectomy.3,26 Other factors that have been
associated with increased risk of emotional distress posthysterectomy include
loss of childbearing capacity, adverse effects on a woman's self-image, social
disruption due to a long recovery time, and history of inadequately dealing
with loss.3,30 The results of a meta-analysis showed that early
detection of ovarian failure, immediate initiation of HT in perimenopausal
women and in those undergoing oophorectomy, and regular follow-up may improve
psychological outcomes of hysterectomy.31
Conclusions
Although
hysterectomy is generally a safe procedure, it is pertinent for pharmacists to
be aware of the surgical, postsurgical, and long-term complications involved.
Educating women concerning the possible complications involved with
hysterectomy may ease patients' preoperative anxiety and ultimately improve
outcomes. Pharmacists have an important role in the care of this population of
women and can aid in the prevention and treatment of complications associated
with hysterectomy by providing proper education, identifying high-risk
patients, and assisting with the management of medications.
REFERENCES
1. Keshavarz H,
Hillis SD, Kieke BA, Marchbanks PA. Hysterectomy surveillance--United States,
1994-1999. MMWR. 2002;51(SS05):1-8.
2. Hysterectomy.
National Women's Health Network Web site. Available at:
www.nwhn.org/content/index.php?pid=133. Accessed July 17, 2006.
3. Falcone R,
Cogan-Levy SL. Overview of Hysterectomy. UpToDate Online 14.2 Web site.
Available at:
www.utdol.com/utd/content/topic.do?topicKey=gyn_surg/11669&type=A&selectedTitle=2~58.
Accessed July 14, 2006.
4. Lefebvre G, Allaire
C, Jeffrey J, et al. SOGC clinical guidelines. Hysterectomy. J Obstet
Gynaecol Can. 2002;24:37-61.
5. Kramer MG, Reiter
RC. Hysterectomy: indications, alternatives and predictors. Am Fam Physician
. 1997;55:827-834.
6. McPherson K,
Metcalfe MA, Herbert A, et al. Severe complications of hysterectomy: the VALUE
study. BJOG. 2004;111:688-694.
7. Garry R, Fountain J,
Mason S, et al. The eVALuate study: two parallel randomised trials, one
comparing laparoscopic with abdominal hysterectomy, the other comparing
laparoscopic with vaginal hysterectomy. BMJ. 2004;328:129.
8. Stovall TG, Mann WJ.
Vaginal Hysterectomy. UpToDate Online 14.2 Web site. Available at:
www.utdol.com/utd/content/topic.do?topicKey=gyn_surg/6246&type=A&selectedTitle=2~7.
Accessed July 14, 2006.
9. Stovall TG, Mann WJ.
Abdominal Hysterectomy. UpToDate Online 14.2 Web site. Available at:
www.utdol.com/application/index/indexResults.asp?index=211494&title=Abdominal%20hysterectomy&order=1~2.
Accessed July 14, 2006.
10. Dandade D, Malinak
LR, Wheeler JM. Therapeutic Gynecologic Procedures. Current Obstetric &
Gynecologic Diagnosis and Treatment. STAT!Ref Online Medical Database.
Available at: online.statref.com/document.aspx?fxid=30&docid=554. Accessed
July 14, 2006.
11. Stovall TG, Mann
WJ. Overview of Laparoscopic Surgery. UpToDate Online 14.2 Web site. Available
at:
www.utdol.com/utd/content/topic.do?topicKey=gyn_surg/10533&type=A&selectedTitle=2~71.
Accessed July 14, 2006.
12. Maresh MJ, Metcalfe
MA, McPherson K, et al. The VALUE national hysterectomy study: description of
the patients and their surgery. BJOG. 2002;109:302-312.
13. van der Vaart CH,
van der Bom JG, de Leeuw JR, et al. The contribution of hysterectomy to the
occurrence of urge and stress urinary incontinence symptoms. BJOG.
2002;109:149-154.
14. Brown JS, Sawaya G,
Thom DH, Grady D. Hysterectomy and urinary incontinence: a systematic review.
Lancet. 2000;356:535-539.
15. Kjerulff KH,
Langenberg PW, Greenaway L, et al. Urinary incontinence and hysterectomy in a
large prospective cohort study in American women. J Urol.
2002;167:2088-2092.
16. Meeks GR, Harris
RL. Surgical approach to hysterectomy: abdominal, laparoscopy-assisted, or
vaginal. Clin Obstet Gynecol. 1997;40:886-894.
17. Croak AJ, Gebhart
JB, Klingele CJ, et al. Characteristics of patients with vaginal rupture and
evisceration. Obstet Gynecol. 2004;103:572-576.
18. Harris WJ.
Complications of hysterectomy. Clin Obstet Gynecol. 1997;40:928-938.
19. Ahn EH, Bai SW,
Song CH, et al. Effect of hysterectomy on conserved ovarian function.
Yonsei Med J. 2002;43:53-58.
20. Rhodes JC, Kjerulff
KH, Langenberg PW, Guzinski GM. Hysterectomy and sexual functioning. JAMA
. 1999;282:1934-1941.
21. Rozenberg S, Caubel
P, Lim PC. Constant estrogen, intermittent progestogen vs. continuous combined
hormone replacement therapy: tolerability and effect on vasomotor symptoms.
Int J Gynaecol Obstet. 2001;72:235-243.
22. Nelson HD.
Assessing benefits and harms of hormone replacement therapy: clinical
applications. JAMA. 2002;288:882-884.
23. Kalantaridou SN,
Davis SR, Calis KA. Hormone therapy in women. In: DiPiro JT, Talbert RL, Yee
GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed.
New York: McGraw-Hill; 2005:1493-1510.
24. Premarin Package
Insert. Philadelphia, PA: Wyeth Pharmaceuticals Inc.; April 2006.
25. Anderson GL,
Limacher M, Assaf AR, et al; Women's Health Initiative Steering Committee.
Effects of conjugated equine estrogen in postmenopausal women with
hysterectomy: the Women's Health Initiative randomized controlled trial.
JAMA. 2004;291:1701-1712.
26. Randomised
comparison of oestrogen versus oestrogen plus progestogen hormone replacement
therapy in women with hysterectomy. Medical Research Council's General
Practice Research Framework. BMJ. 1996;312:473-478.
27. Hickey M, Davis SR,
Sturdee DW. Treatment of menopausal symptoms: what shall we do now? Lancet
. 2005;366:409-421.
28. Roovers JP, van der
Bom JG, van der Vaart CH, Heintz AP. Hysterectomy and sexual wellbeing:
prospective observational study of vaginal hysterectomy, subtotal abdominal
hysterectomy, and total abdominal hysterectomy. BMJ. 2003;327:774-778.
29. Thakar R, Ayers S,
Clarkson P, et al. Outcomes after total versus subtotal abdominal
hysterectomy. N Engl J Med. 2002;347:1318-1325.
30. Wright JB, Gannon
MJ, Greenberg M. Psychological aspects of heavy periods: does endometrial
ablation provide the answer? Br J Hosp Med. 1996;55:289-294.
31. Khastgir G, Studd
JW, Catalan J. The psychological outcome of hysterectomy. Gynecol Endocrinol
. 2000;14:132-141.
To comment on this article, contact
editor@uspharmacist.com.






