US Pharm. 2007;32(8):22-26.
In the United States, suicide ranks 11th among causes of death.1 While there is an underestimation of the true incidence of suicidal behavior, it is the third leading cause of mortality among individuals ages 15 to 24. The highest rate of death by suicide is among men 75 or older; elderly white men are at highest risk. Male suicide deaths outnumber female deaths by four to one among all age groups.1
Although seniors in the U.S. constituted only 12% of the population in 2004, they accounted for 16% of suicide deaths.2 In older Americans, geriatric depression is one of the most common conditions associated with completed suicide.3-6 This is a considerable concern for health care practitioners, since of the 33 million Americans ages 65 and older, five million are reported to suffer from serious and persistent symptoms of depression and an additional one million are diagnosed with clinical or major depression.7
Suicidal ideation, defined as thoughts and plans about suicide, is considered distinct from suicidal behavior, which includes three types of self-destructive acts: a suicidal gesture (an act with a very low lethal potential), attempted suicide (an act intended to be self-lethal that does not result in death), and completed suicide (a suicidal act resulting in death).1 Suicidal ideation and gestures should be taken seriously, as they are considered an unmistakable communication of desperation, hopelessness, or pleas for help from individuals who still want to live.1,8 It is approximated that more than 700,000 suicide attempts occur annually, with many individuals making repeated attempts; 10% of those attempting suicide eventually succeed. Suicide attempts, while more rare in seniors than in younger individuals, are more lethal in the elderly as a result of fewer indications of the intent, more lethal self-destructive acts, and more careful planning.9
Seeking out or responding to suicide interventions is more likely to occur in a younger patient as opposed to a senior.10 The rates of attempted and completed suicides are higher among those who live alone (i.e., as a result of separation, divorce, or spouse's death), and married people of both genders have a considerably lower suicide rate than do single people.
Primary Remediable Risk Factor in
Suicide
The primary risk factor for suicide, which is considered to be remediable, is
depression. Depression is one of the most common psychiatric disorders among
all seniors, with approximately one third of seniors in institutionalized
settings exhibiting clinically significant depressive symptoms.10
Although mood disorders are more prevalent in women than in men of all ages,
completed suicide is disproportionately higher in males, especially in elderly
men.9 Additional factors associated with suicide include use of
alcohol and drugs of abuse, schizophrenia, personality disorders, aggression,
and physical disorders (Table 1). The use of alcohol intensifies
depression, thereby increasing the likelihood of suicide; persistent and
excessive drinking can even lead to remorseful feelings and suicidal behavior,
even during sober periods.8
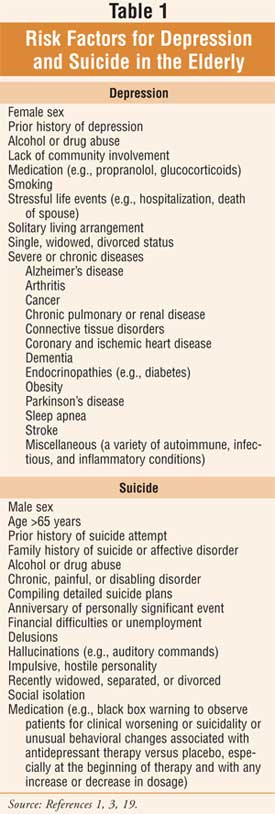
Patients with a medical condition are twice as likely to develop depression, and some conditions, such as alcoholism and drug dependency, are associated with a higher prevalence and persistence of depression (Table 2). Depression worsens the outcomes of medical disorders and increases mortality in hospitalized patients.9,11 Among the elderly, serious physical conditions (e.g., chronic, severe, painful) are considered contributory in about 20% of suicide cases.1
Role of the Pharmacist
Pharmacists should closely monitor all patients with chronic
medical problems for signs and symptoms of depression, which may include
depressed mood; decreased interest or pleasure in activities; changes in
appetite, weight, or sleep; psychomotor agitation or retardation; loss of
energy; inability to concentrate; indecisiveness; and thoughts of death,
dying, or suicide. In the depressed elderly, apathy, withdrawal, and somatic
complaints (e.g., complaints of vague aches and pains) are often the
presenting signs, compared with the psychological complaints often reported by
younger patients. The Geriatric Depression Scale, available in a variety of
languages, is an assessment tool that is utilized in identifying seniors who
require further evaluation or referral for depression (Table 2).
12,13
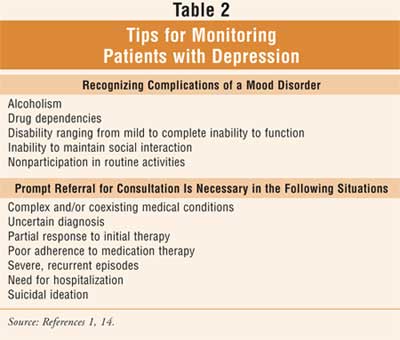
Pharmacists should be aware that the majority of people seeking assistance for psychological distress reach out to their primary care provider, as opposed to a mental health specialist, and more than half of psychiatric patients receive care exclusively in the primary care setting.14,15 This is an important point, since approximately 75% of elderly individuals who die by suicide visited their primary care physician within the month prior to their deaths.2,10,16Pharmacists should work at improving the detection and treatment of depression toward the goal of reducing suicide risk.
The underdiagnosis and undertreatment of depression may be attributed to a variety of misconceptions held by both the patient and clinician.3,17 It must be noted that excessive fatigue, changes in appetite, or escalating irritability that causes isolation is not part of the natural aging process and therefore should not be attributed to such.3,7 Additionally, while depression may be a risk factor for dementia, it can also appear as a prodrome of dementia or exist comorbidly with dementia.3
Pharmacologic Intervention for
Depression
In order to overcome geriatric depression, well-tolerated, effective therapy
is recommended, including:
1. antidepressants (e.g., selective
serotonin reuptake inhibitors, tricyclic antidepressants [TCAs], monoamine
oxidase inhibitors, and miscellaneous agents);
2. electroconvulsive therapy;
3. cognitive behavioral therapy and problem-solving therapy (especially with
executive dysfunction);
4. bibliotherapy (reading self-help literature); and
5. wellness adjuncts (e.g., exercise).17
Although it is beyond the scope of this article to discuss the pharmacologic management of depression in depth, more information can be found in the review article "Depression in the Elderly" by Birrer et al. 3 Tailoring the choice of an antidepressant agent to the individual and utilizing an adequate dosage and trial period (e.g., 6-12 weeks) are essential in the treatment of depression in the elderly.3,9 Physical changes (e.g., to renal, hepatic, or cardiac function) and medical conditions associated with aging have a pharmacokinetic and pharmacodynamic impact on medication therapy. The increased risk of adverse medication effects (e.g., anticholinergic burden, risk of falling secondary to orthostatic hypotension) must be understood with regard to geriatric dosage guidelines (start low, go slow), disease–drug contraindications (e.g., cardiac conduction defects and TCAs), and drug interactions (e.g., possible toxicities associated with cytochrome P-450 inhibition).
Goals of pharmacologic treatment include improved family and social functioning, decreased discomfort, and significant improvement in satisfaction with life in general; determining adequate treatment response may be guided by improvement in sleep, appetite, energy, and attitude.18 Full therapeutic response generally requires months of pharmacologic intervention; however, a partial response may be seen in three to four months.
Summary
The primary risk factor for suicide is depression. While seniors with a
medical condition are twice as likely to develop depression, it is often
underrecognized and undertreated. Since geriatric depression is one of the
most common conditions associated with completed suicide in the U.S.,
pharmacists should be attentive and astute in monitoring these individuals.
Pharmacists should monitor all seniors with chronic medical conditions, especially those conditions associated with a higher prevalence and persistence of depression, for signs and symptoms that may indicate the need for treatment intervention. Through a process of ongoing assessment using tools specifically designed for the geriatric population, pharmacists can contribute to the urgent need for early detection and treatment intervention for depression and, potentially, impact the risk of suicide in this vulnerable population.

References
1. Beers MH, Berkow R. The Merck Manual of Diagnosis and Therapy. 17th
ed. Whitehouse Station, NJ: Merck & Co.;1999:1703-1717,1741-1744.
2. Older adults: depression and suicide facts. National Institute of Mental
Health. 2003. Pub. No. 03-4593. Available at: www.nimh.nih.gov. Accessed July
8, 2007.
3. Birrer RB, DeLisi M, Dadoyan TA. Depression in the elderly. P&T.
2007;32:168-180.
4. Erickson K, Drevets W, Schulkin J. Glucocorticoid regulation of diverse
cognitive functions in normal and pathological emotional states. Neurosci
Biobehav Rev. 2003;27:233-246.
5. Ballmaier M, Sowell ER, Thompson PM, et al. Mapping brain size and cortical
gray matter changes in elderly depression. Biol Psychiatry.
2004;55:382-389.
6. Alexopoulos GS. Depression in the elderly. Lancet.
2005;365:1961-1970.
7. Depression in older persons. National Association of Mental Illness. 2003.
Available at: www.nami.org. Accessed July 8, 2007.
8. Beers MH, Jones TV, Berkwits M, et al., eds. The Merck Manual of Health
& Aging. Whitehouse Station, NJ: Merck Research Laboratories;
2004:390,888.
9. Apfeldorf WJ, Alexopoulos GS. Late-life mood disorders. In: Hazzard WR,
Blass JP, Halter JB, et al. Principles of Geriatric Medicine and Gerontology
. 5th ed. New York, NY: McGraw-Hill, Inc; 2003:1443-1458.
10. Beers MH, Berkow R., eds. The Merck Manual of Geriatrics. 3rd ed.
Whitehouse Station, NJ: Merck & Co; 2000:310-322,1167,1171-1174.
11. Zagaria ME. Depression in older male patients. U.S. Pharmacist.
2006;31(8):34-40.
12. Geriatric Depression Scale. Available at:
www.stanford.edu/~yesavage/GDS.html. Accessed July 9, 2007.
13. Geriatric Depression Scale (GDS) Fact Sheet. Available at:
www.patienttools.com/v3/assess_GDS.asp. Accessed July 9, 2007.
14. Landis BJ, Marsh CC. Mental health disorders. In: Youngkin EQ,
Sawin KJ, Kissinger JF, et al. Pharmacotherapeutics: A Primary Care Guide
. Upper Saddle River, NJ: Pearson Prentice Hall; 2005:709-750.
15. Afinson TJ, Bona JR. A health services perspective on delivery of
psychiatric services in primary care including internal medicine. Med Clin
North Am. 2001;85:597-616.
16. Kane RL, Ouslander JG, Abrass IB. Essentials of Clinical Geriatrics
. 4th ed. New York, NY: McGraw-Hill, Inc.;1999:3-17,154-180,512,623.
17. Blazer DG. Depression in late life: review and commentary. J Gerontol A
Biol Sci Med Sci. 2003;58:249-265.
18. Oxman TE, Hull JG. Social support and treatment response in older
depressed primary care patients. J Gerontol. 2001:35-45.
19. Semla TP, Beizer JL, Higbee MD. Geriatric Dosage Handbook. 12th ed.
Hudson, Ohio: Lexi-Comp, Inc.; 2007.
To comment on this article, contact editor@uspharmacist.com.





