US
Pharm. 2006;4:54-62.
With the rise in popularity
and success of radical weight-loss surgery among obese persons, a new
postoperative cosmetic challenge has emerged. Following massive weight loss
achieved by diet, exercise, gastric bypass, or gastric banding, the patient
typically has significant areas of excess skin, commonly including on the
abdomen, breasts, arms, and thighs. Skin will progressively sag in
characteristic as well as idiosyncratic patterns like melting wax from a
burning candle. No amount of exercise or special diets will tighten it. Total
body lift surgery addresses the entire skin laxity problem of the trunk and
thighs. The transverse removal of unwanted skin and fat is followed by tight
closure, which in effect lifts the lower adjoining region. While the
improvements are dramatic, this is major surgery that comes with serious risks
and impressive scars.

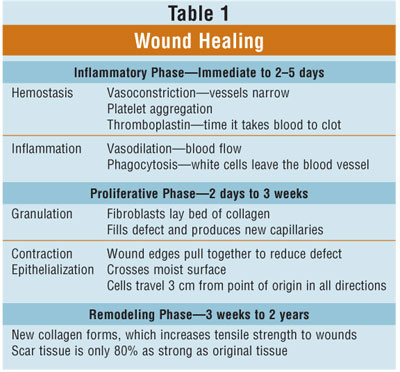
Wound Healing
The wound healing
process (TABLE 1) is a complex series of events that begin at the moment of
injury and continue for months to years. A thin coagulum of fibrin (from the
tissues and serum) and red blood cells forms a clot that unites the edges of
the wound. Eventually the clot is replaced by granulation tissue, a connective
tissue with a rich blood supply. Scars are red because of increased small
vessels, and the color gradually fades to white as the vascularization
decreases and the collagen matrix matures. Remodeling of the collagen matrix
may continue for years depending on individual genetics and age. In general, a
thin pale long scar remains when the scars are mature.
Many variables can affect the
severity of scarring, including the size and depth of the wound, the blood
supply to the area, the thickness and color of the skin, and the direction of
the scar. How much the appearance of the scar bothers a patient is, of course,
a personal matter. While no scar can be removed entirely, its appearance can
be improved. The de gree of improvement depends on the size and direction of
the scar, the nature and quality of the person's skin, and how well the person
cares for the wound after the operation.
Two Types of Scars
Keloids are
thick, puckered, itchy clusters of scar tissue that grow beyond the edges of
the wound or incision. They are often red or darker in color than the
surrounding skin. Keloids occur when the body continues to produce the tough,
fibrous protein known as collagen, after a wound has healed. Keloids can
appear anywhere on the body, but they are most common over the breastbone, on
the earlobes, and on the shoulders. They occur more often in dark-skinned
people than in those who are fair-skinned. The tendency to develop keloids
lessens with age. Hypertrophic scars are often confused with keloids, since
both tend to be thick, red, and raised. Hypertrophic scars, however, remain
within the boundaries of the original incision or wound.
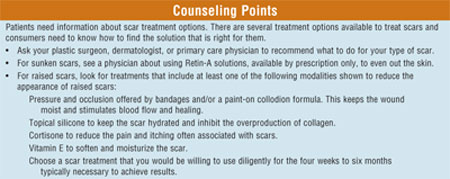
Treatment Methods
Keloids can be treated
aggressively and early by injecting a steroid medication directly into the
scar tissue to reduce redness, itching, and burning. In some cases, this will
also shrink the scar. If steroid treatment is inadequate, the scar tissue can
be cut out and the wound closed with one or more layers of stitches. This is
generally performed under local anesthesia as an outpatient procedure, and
stitches are removed in a few days. Unfortunately, keloids tend to recur,
sometimes larger than before. In some cases, application of a pressure garment
over the area is recommended for as long as a year. Keloids may return at any
time, requiring repeated procedures, but this is not common.
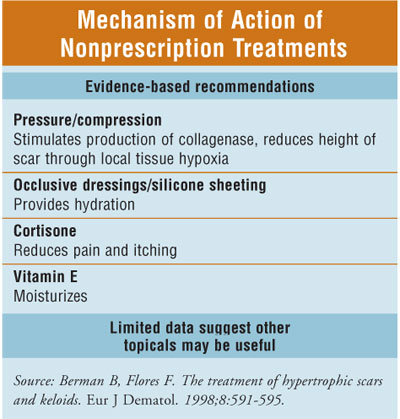
Hypertrophic scars often improve
on their own--though it may take a year or more with the help of steroid
applications or injections. If a conservative approach does not appear to be
effective, hypertrophic scars can often be improved surgically. The plastic
surgeon will remove excess scar tissue and may reposition the incision so that
it heals in a less visible pattern. The surgery may be done under local or
general anesthesia, depending on the scar's location and what the patient and
surgeon decide. The patient may receive steroid injections during surgery and
at intervals for up to two years afterward to prevent the thick scar from
forming again.
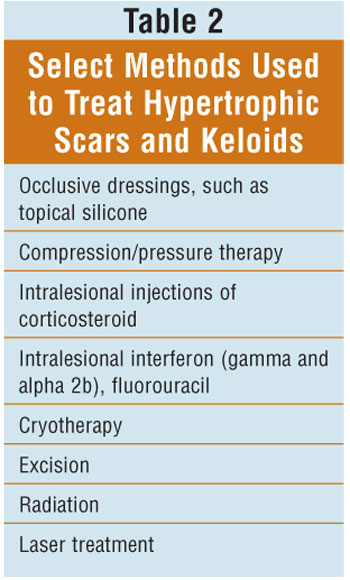
Differentiating hypertrophic scars
from keloids can be challenging. Scars can range between those that become
hypertrophic in the first few months and then completely resolve with no
treatment, to the keloids that become disfiguring and permanent. Table 2 shows
methods used to treat scars.
Silicone gel sheeting has been a
widely used option for hypertrophic scars and keloids since the 1980s. The
mechanism of action of topical silicone is unknown but there are temperature
differences as small as 1°C under silicone gel sheeting. This could have a
profound effect on collagen kinetics and may reduce scarring. Silicone itself
has never been found in significant amounts in scars treated with sheeting, so
a direct chemical effect is unlikely. It has also been theorized that static
electricity generated by silicone gel sheeting induces a polarization of scar
tissue that results in involution. Occlusion of scars by silicone gel sheeting
might alter cytokine levels, which in turn would have an effect on scar
remodeling (Figure 1).
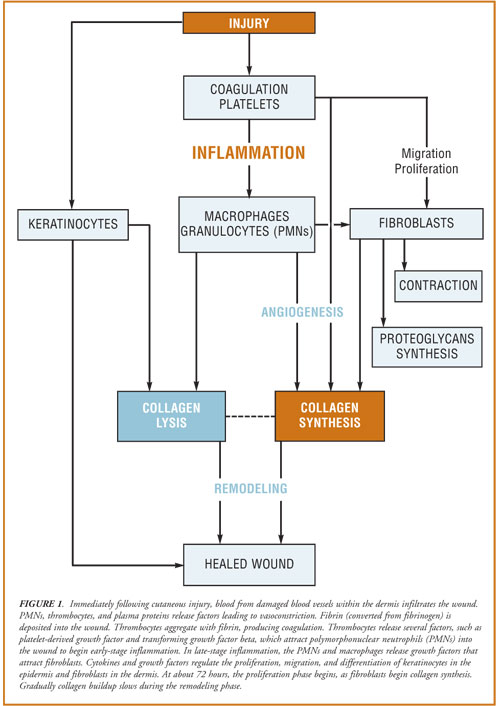
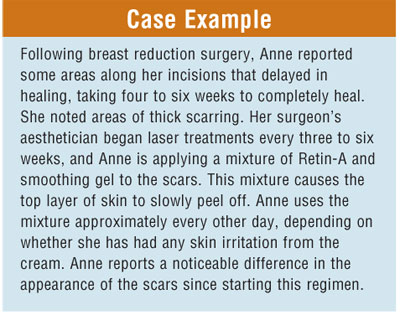
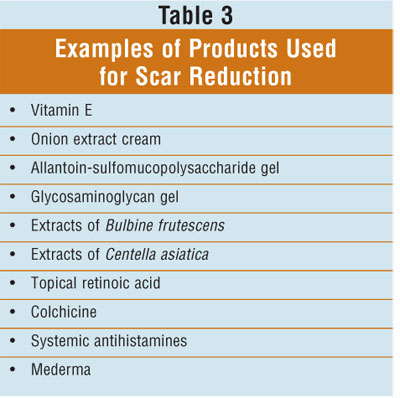
Table 3 lists additional
treatments that can be used to improve the appearance of scars. If the scar
requires more intensive treatment, additional options include dermabrasion,
scar revision surgery, cortisone injections, cryosurgery, and laser
resurfacing. A useful graded protocol to manage postoperative scarring starts
with patients using silicone gel sheeting at three to four weeks. The
application of adhesive microporous hypoallergenic paper tape after surgery is
frequently successful. The mechanism of benefit is unknown, but it may in part
be mechanical (pressure) and/or occlusive.
Adapted from Total Body Lift by
Dennis J. Hurwitz, MD, FACS, Director, Hurwitz Center for Plastic Surgery,
Pittsburgh, Pennsylvania.
To comment on this article,
contact editor@uspharmacist.com.






