Osteoarthritis is a common
rheumatologic disorder. It is characterized by a gradual loss of cartilage
from the joints and, in some people, joint inflammation. Symptoms of
osteoarthritis include pain, stiffness, and loss of joint motion. It is
estimated that 40 million Americans of all ages are affected by osteoarthritis
and that 70% to 90% of Americans older than 75 have at least one joint
involved.1 In the United States, women are more often affected by
osteoarthritis, and older women are twice as likely to be affected by
osteoarthritis of the hands and knees than comparably aged men.2 As
the population of elderly patients continues to grow, osteoarthritis becomes a
significant medical and financial concern. With recent issues surrounding
NSAIDs and cyclooxygenase-2 (COX-2) inhibitors, managing osteoarthritis is now
more complex and individualized. This article briefly discusses the
background, prevalence, and diagnosis of osteoarthritis, then focuses on the
treatment options available for this disease.
PREVALENCE
The number of
osteoarthritis cases rises in people of advancing age, possibly beginning as
early as the third decade of life. The exact prevalence is unknown due to
uncertainties and variations in diagnostic definitions and reports of this
disease. In Western countries, radiographic change evident of osteoarthritis
is present in the majority of people by 65 years of age and in about 80% of
people older than 75.3 Notably, structural changes are not
necessarily associated with clinical symptoms of pain and inflammation. Many
patients with radiographic changes are asymptomatic, and those with symptoms
of osteoarthritis may not have evidence of radiographic changes of the
affected joint. Thus, an accurate diagnosis should consider the patient's
history, physical exam, and radiographic findings.
PATHOPHYSIOLOGY
The
pathophysiology of osteoarthritis involves mechanical, biochemical, and
cellular processes. The common pathway is that all these processes change the
composition and properties of articular cartilage. Synovial fluid, along with
articular cartilage, permits almost frictionless movement of joint bones at
their points of contact. Healthy cartilage allows internal remodeling as
chondrocytes replace macromolecules lost in degradation. This process is
disrupted in osteoarthritis and is characterized by a progressive
deterioration of cartilage, resulting in the formation of osteophytes and loss
of cartilage.
Early changes to the joints
do not result in any symptoms, since there are no nerve fibers in articular
cartilage. Potential sources of pain in osteoarthritis include denuded bone,
microfractures of bone, stress to ligaments due to loss of cartilage,
low-grade synovitis, and spasms of surrounding muscles as the disease
progresses.
CAUSES AND CLINICAL FEATURES
The precise cause
of osteoarthritis is unknown. Multiple factors, such as heredity, trauma, and
obesity, interact to cause this disorder. Osteoarthritis is not a systemic
disease, and joint distribution often occurs in the knees, hands, and hips;
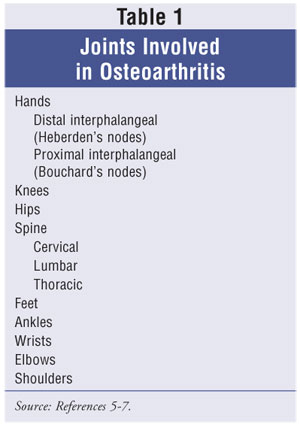
however, other joints can also be affected. Table 1 lists joints often
affected by osteoarthritis. Osteoarthritis tends to develop slowly and
progresses over several years. The pain is often described as aching and is
felt in the areas surrounding the affected joint. Bony enlargements and
irregularities are typical, especially in the hands at the distal
interphalangeal joints (Heberden's nodes) and less commonly in the proximal
interphalangeal joints (Bouchard's nodes). Although these bony enlargements
are asymptomatic, many patients view them as part of a disabling arthritic
disorder or even an outward sign of aging. The clinical presentation of
osteoarthritis depends on the number of joints affected and the duration and
severity of the disease.
Patients with osteoarthritis of
the hip may complain of gait problems. After a period of inactivity, hip
stiffness is common and is usually a presenting factor. Patients with
osteoarthritis that affects the hands often have problems with manual
dexterity. This is evident when the first carpometacarpal joint is involved.
Instability or buckling of the knee is often noted in patients with knee
osteoarthritis. Some patients with erosive osteoarthritis may have signs of
inflammation in the interphalangeal joints of the hands. However,
osteoarthritis generally does not carry an inflammatory component, except in
severe, advanced disease.
Radiographic features and
laboratory findings are not definitive in the diagnosis of osteoarthritis.
Radiographic features of the disease show loss of joint space and presence of
new bone formation or osteophytes. However, absence of these radiographic
changes does not exclude a diagnosis of osteoarthritis. Analysis of synovial
fluid tends to reveal a white blood cell count of less than 2,000 per
millimeter.4
DIAGNOSIS
Diagnosis is
often made through physical examination and a detailed history of symptoms.
The American College of Rheumatology (ACR) has diagnostic criteria for
osteoarthritis at various sites, including the hip, knee, and hand.5-7
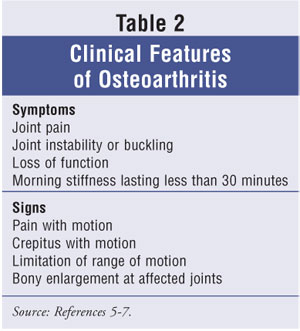
The usual presenting symptom is pain involving one or a few joints, but joint
involvement is usually asymmetric. Patients may complain of morning joint
stiffness that resolves within 30 minutes, which distinguishes osteoarthritis
from rheumatoid arthritis. As the disease progresses, joint stiffness can be
prolonged, and crepitus--a grating sensation in the joint--can occur. Crepitus
is caused by irregularities of the joint surfaces. Table 2 lists clinical
features of osteoarthritis.
TREATMENTS
The goals of
treatment for osteoarthritis are to control pain and swelling, minimize
disability, improve the quality of life, and educate patients about their role
in disease management. Treatment should be individualized to the patient's
level of function and activity, expectations, occupational needs, joints
involved, and disease severity, and to any coexisting medical problems.
Nonpharmacological Treatment
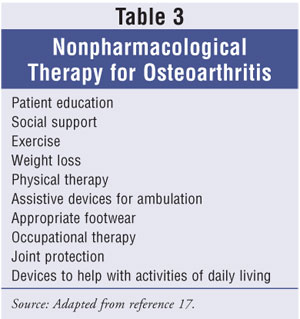
Nonpharmacologic
treatment, e.g., patient education, exercise programs, weight loss, assistive
devices, and alternative therapy supplements, appears to be the foundation for
management of this disease. Educational materials for patients to better
understand their diagnosis can be obtained from the Arthritis Foundation
(www.arthritis.org). Table 3 provides examples of nonpharmacological therapy
for osteoarthritis.
Patient Education: Education about the causes, effects, and symptoms of osteoarthritis, as well as a realistic understanding of what can be achieved with optimal therapy, is essential. Osteoarthritis has both physical and psychological effects. Its symptoms and limitations may cause feelings of frustration, dependency, and even depression. The more patients learn about the disease, the more they can participate in their own care. Social support can be achieved by building an informal support team or by participating in formal osteoarthritis groups.
Exercise
Programs: The goals of an exercise program are to maintain range of
motion, muscle strength, and general health. Patients with osteoarthritis are
often concerned that using a joint will "wear out" the already damaged area.
However, evidence shows that patients with osteoarthritic joints who
participated in regular low-impact exercise (e.g., biking and elliptical
machines) did not have an increased development of osteoarthritis.8
Patients should be encouraged to participate in aerobic exercises, such as
swimming or walking. Exercise can help combat the depression that may
accompany the chronic pain of osteoarthritis.9
Weight Loss:
Although obesity appears to be a greater risk factor for women, an association
exists between obesity and osteoarthritis of the knee in both genders.10
Weight loss has been shown to benefit patients with osteoarthritis.11
Symptoms associated with arthritis in the hips, knees, and feet are
exacerbated by obesity. Thus, primary prevention strategies should include
measures to achieve weight loss or avoid weight gain in overweight patients.
Assistive Devices:
A variety of appliances can help relieve osteoarthritis symptoms by
supporting the muscles linked to the affected joint. Examples of assistive
devices include crutches, walking aids, shoes inserts, splints, braces, and
special soles.11 Using special appliances may help patients feel
more comfortable, move around independently, and have improved function.
Physical and occupational therapy
may benefit patients with specific physical disabilities brought on by
osteoarthritis. Incorporating individualized exercise programs and teaching
patients how to manage activities of daily living may lead patients to feel
more independent and less affected by their disease.
Alternative Therapy
Supplements: Patients often seek alternative therapies for
osteoarthritis after experiencing side effects or incomplete relief of
symptoms from conventional medications. Since the herbal and supplement
industry is not regulated by the FDA, supplement composition can vary.
Glucosamine sulfate, a
popular treatment for osteoarthritis symptoms, is derived from oyster and crab
shells. No published studies have documented arthroscopic improvement in
arthritic cartilage with glucosamine use in humans. A meta-analysis concluded
that glucosamine may show efficacy over placebo in relieving painful symptoms.
12 Glucosamine is usually dosed at 1,500 mg per day in three divided
doses. Supplements should be taken for at least a month before improvement
occurs.
Chondroition sulfate has
demonstrated efficacy by acting as a building block of proteoglycan molecules
to improve the symptoms of osteoarthritis.13 Chondroitin is derived
mostly from shark and cow cartilage. Chondroitin is usually dosed at 1,200 mg
per day in three divided doses, and results may not be achieved for at least a
month.
Little evidence exists
showing that the combination of glucosamine and chondroitin is more effective
than either supplement alone.14 However, the use of the two
together is popular for the treatment of osteoarthritis. The
Glucosamine/Chondroitin Arthritis Intervention Trial (GAIT) was a six-month,
five-arm trial involving 1,500 osteoarthritis patients with mild to severe
pain. Patients were given glucosamine, chondroitin, glucosamine and
chondroitin combined, celecoxib, or placebo daily. The GAIT abstract posted on
the ACR Web site concludes that glucosamine and chondroitin together are
beneficial in treating moderate to severe knee pain due to osteoarthritis.
Results have yet to be presented.
S-adenosylmethionine (SAMe)
is a naturally occurring compound found in all living cells that is
commercially produced in yeast-cell cultures. Several studies have found SAMe
to be more effective than placebo in improving pain and stiffness related to
osteoarthritis.15,16 Dosages range from 400 to 1,200 mg per day.
Pharmacological Treatment
At present, there
are no specific pharmacologic therapies that can prevent the progression of
joint damage due to osteoarthritis. Because no medication has been shown to
cure this disease, patients should clearly understand the risks and benefits
of their treatment options. Pain relief is the primary indication for the use
of pharmacologic agents in patients with osteoarthritis who do not respond to
nonpharmacologic interventions. When quality of life becomes affected, it
would be appropriate to initiate pharmacotherapy to minimize disability and
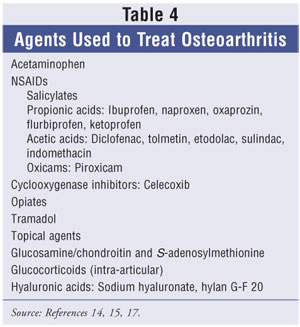
control pain. This article focuses on analgesics, NSAIDs, COX-2 inhibitors,
and intra-articular glucocorticoids and hyaluronate. Table 4 provides a list
of agents used to treat osteoarthritis.
Analgesics, NSAIDs, and COX-2
Inhibitors: The nonprescription analgesic acetaminophen, at doses of 1,000 mg
four times a day or 650 mg every four hours (up to a maximum of 4 g/day), is
the drug of choice for pain relief for noninflammatory osteoarthritis. The ACR
guidelines emphasize the use of acetaminophen as first-line treatment for
osteoarthritis of the knee and hip.17 This analgesic can
significantly improve function and decrease pain. Therapeutic doses of
acetaminophen produce minimum adverse effects, but hepatotoxicity can occur,
especially in patients who consume large quantities of alcohol.
NSAIDs are appropriate
choices for treating moderate or severe arthritis pain, as well as the
swelling, stiffness, and warmth of inflammation when present. NSAIDs carry a
risk of gastrointestinal (GI) toxicity, even at a low dose. GI complications
occur over the course of one year in about 2% to 4% of patients, and incidence
increases with age.9 Reduced prostaglandins in the gastric mucosa
from COX inhibition attributes to the GI side effects of NSAIDs. Proton pump
inhibitors may help control the GI symptoms associated with chronic NSAID use.
Misoprostol, a synthetic prostaglandin E1, can help prevent gastric
ulcers in patients on long-term NSAID therapy. Several risk factors appear to
increase the risk of NSAID-induced toxicity, especially in patients over age
65; patients with previous ulcer or upper GI bleeding; and patients taking
concomitant oral cortico steroids, anticoagulants, or multiple NSAID therapy.
18 The ACR guidelines recommend starting NSAIDs at low analgesic doses
and increasing to full anti-inflammatory doses only if the lower dose did not
provide adequate relief.17 The concurrent use of acetaminophen with
NSAIDs may allow the NSAID dosage to be reduced, thereby limiting toxicities.
COX-2 inhibitors may be
appropriate to initiate for patients with moderate to severe pain when non
selective COX inhibitors have proven ineffective or for those patients who
have a history of GI disease. COX-2 inhibitors have at least a 200- to
300-fold selectivity for inhibition of COX-2 over COX-1. Celecoxib is
recommended in doses of 200 mg per day for the treatment of osteoarthritis
pain. COX-2 inhibitors are associated with lower gastroduodenal toxicity, but
an increased risk of cardiovascular events has led to the withdrawal of two
previous agents (rofecoxib and valdecoxib) from the market. Although elderly
patients may choose to use celecoxib because of less GI effects, they need to
be made aware of the risks and benefits by their physician before beginning
treatment.
Treatment options for
osteoarthritis have been further complicated by the potential cardiovascular
risk associated with the use of naproxen and other NSAIDs. All NSAIDS, both
over-the-counter and prescription, and COX-2 inhibitors carry a warning
regarding cardiovascular and GI risks.19
Tramadol is usually given as
a rescue medication for symptomatic relief and can be considered an option if
NSAIDs fail. Use of this central-acting oral analgesic allows for a lower dose
of NSAIDs to be used. The recommended dose is 50 mg given every four to six
hours, with a total daily dose not exceeding 400 mg.9 Opioids can
be considered for patients with severe osteoarthritic pain that does not
respond to nonopioid analgesic agents. These agents are not recommended for
prolonged time periods because they cause constipation and increase the fall
risk, especially in the elderly.
Topical capsaicin, a
pepper-plant derivative, has been shown to relieve pain relating to
osteoarthritis better than placebo. Capsaicin cream 0.025% applied four times
a day was effective in managing pain caused by osteoarthritis of the knee,
ankle, wrist, and shoulder in a double-blind, randomized, controlled trial.
20 One common side effect is a localized burning sensation, and patients
should be advised to wash hands after application to avoid spreading to the
eyes or other mucous membranes. Capsaicin is available over the counter in
concentrations of 0.025%, 0.075%, and 0.25%.
Intra-Articular
Glucocorticoids and Hyaluronate: Patients who suffer from painful
flares of osteoarthritis in the knee may benefit from intra-articular
injections of corticosteroids, such as methylprednisolone or triamcinolone.
Short-term pain relief can be obtained with aspiration of the joint fluid,
followed by intra-articular injection of the corticosteroid when the joint is
painful and swollen. Injections should not be made in the joints more than
three or four times a year, to prevent potential cartilage damage from
repeated injections. Patients may have to consider surgical intervention if
they require more than three to four shots per year to control symptoms.
Hyaluronic acid provides
viscoelastic and lubricating properties to the joint. It is a major
nonstructural component of the synovial and cartilage matrix makeup. The
molecular weight and concentration of hyaluronic acid is thought to be
decreased in patients with osteoarthritis. The FDA has approved hylan G-F 20
and sodium hyaluronate injections for the treatment of pain caused by
osteoarthritis of the knee. The 2-mL dose is injected once weekly for three
and five weeks, respectively. The injections are well tolerated; however,
local skin reactions and pain with injection have been shown.
Intra-articular injections
must be administered using the aseptic technique, and the aspirated joint
fluid should be examined to rule out infections. Patients should minimize
activity and stress on the joint for several days following an intra-articular
injection.
Surgery
Osteoarthritis
often progresses to a degree where no cartilage remains and bone is rubbing on
bone. These patients who have symptoms that are not controlled with
pharmacologic or nonpharmacologic therapy and who have moderate to severe pain
and functional impairment may be candidates for orthopedic surgery. Depending
on the joint involved, some replacement procedures have become almost routine.
Patients should understand all the risks and benefits of orthopedic surgery
before making a decision.
Conclusion
Osteoarthritis is
a common, slowly progressive disorder that affects the body's joints.
Treatment of osteoarthritis should focus on the minimization of pain and loss
of function. An individualized approach is best for all aspects of the
disease, and the goals of the patient should be considered before selecting a
treatment plan. Nonpharmacologic therapy is the foundation of care for this
disease, and new therapies may become available to prevent further joint
progression in the future. It is important for providers to address with
compassion and understanding both the physical and emotional concerns these
patients may have.
REFERENCES
1. Oddis CV. New
perspectives on osteoarthritis. Am J Med. 1996;100:S10-S15.
2. Solomon L.
Clinical features in osteoarthritis. In: Kelly WN, Harris ED, eds. Textbook of
Rheumatology. 6th ed. Philadelphia: Saunders; 2001:1409-1418.
3. Lawrence RC,
Hochberg MC, et al. Estimates of the prevalence of selected arthritic and
musculoskeletal diseases in the United States. J Rheumatol. 1989;16:427-441.
4. Pelletier JP,
DiBattista, et al. Cytokines and inflammation in cartilage degradation. Rheum
Dis Clin North Am. 1993;19:545-568.
5. Altman R, Alarcon
G, et al. The American College of Rheumatology criteria for classification and
reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505-514.
6. Altman R, Asch E,
et al. The American College of Rheumatology criteria for classification and
reporting of osteoarthritis of the knee. Arthritis Rheum. 1986;29:1039-1049.
7. Altman R, Alarcon
G, et al. The American College of Rheumatology criteria for the classification
and reporting of osteoarthritis of the hand. Arthritis Rheum.
1990;33:1601-1610.
8. Lane NE. Exercise:
a cause of osteoarthritis. J Rheumatol. 1995;22:3-6.
9. DeAngelo NA,
Gordin V. Treatment of patients with arthritis-related pain. J Am Osteopath
Assoc. 2004;104:2-5.
10. Felson DT,
Anderson JJ, et al. Obesity and knee osteoarthritis. The Framingham Study. Ann
Intern Med. 1988;109:18-24.
11. Ravaud P.
Non-drug treatments for osteoarthritis. Presse Med. 2002;31:4S10-4S12.
12. McAlindon TE,
LaValley MP, et al. Glucosamine and chondroitin for treatment of
osteoarthritis: a systematic quality assessment and meta-analysis. JAMA.
2000;283:1469-1475.
13. Bourgeois P,
Chales G, et al. Efficacy and tolerability of chondroitin sulfate 1200 mg/day
vs chondroitin sulfate 3 x 400 mg/day vs placebo. Osteoarthritis Cartilage.
1998(supple A);6:25-30.
14. Kelly GS. The
role of glucosamine sulfate and chondroitin sulfate in the treatment of
degenerative joint disease. Altern Med Rev. 1998;3:27-39.
15. Di Padova C.
S-adenosylmethionine in the treatment of osteoarthritis: review of the
clinical studies. Am J Med. 1987;83:60-65.
16. Bradley JD,
Flusser D, et al. A randomized, double blind, placebo controlled trial of
intravenous loading with S-adenosylmethionine (SAM) followed by oral SAM
therapy in patients with knee osteoarthritis. J Rheumatol. 1994;21:
905-911.
17. Recommendations
for the medical management of osteoarthritis of the hip and knee: 2000 update.
American College of Rheumatology Subcommittee on Osteoarthritis Guidelines.
Arthritis Rheum. 2000;43:1905-1915.
18. Lichtenstein DR,
Syngal S, Wolfe MM. Nonsteroidal anti-inflammatory drugs and the
gastrointestinal tract: a double-edged sword. Arthritis Rheum. 1995;38:5-18.
19. Olsen NJ.
Tailoring arthritis therapy in the wake of the NSAID crisis. N Engl J Med.
2005;352:2578-2580.
20. Altman RD, Auen
A, Holmburg CE. Capsaicin cream 0.025% as monotherapy for osteoarthritis: a
double-blind study. Semin Arthritis Rheum. 1994;23:S25-S33.
To comment on this article,
contact editor@uspharmacist.com.






