US
Pharm. 2006;1:12-15.
The cough and cold market
presents problems for the pharmacist and patient alike for several reasons.
Cough and cold cause significant morbidity in the American population.1,2
Furthermore, manufacturers offer an overwhelming number of products in many
categories, such as decongestant/antihistamine combinations. Several
manufacturers use line-extension strategies to sell products, a tactic that
fosters confusion because the consumer is presented with many products bearing
the parent product's name, e.g., Alka-Seltzer, Benadryl, or Sudafed. The use
of single-entity products versus combinations has also been troublesome for
patients. In addition, the products often undergo dramatic changes, as is
currently the case with many products that formerly contained pseudoephedrine
being reformulated and a new set of antitussive products that include
diphenhydramine. The FDA issues preliminary and final rules that require
profound changes in composition and labeling, as shown in a recent document
concerning sinus labeling, which is described in a later section of this
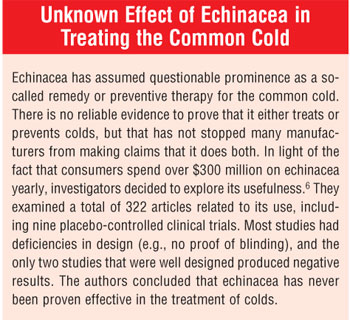
column. Finally, the advent of unproven therapies has clouded the issue of
treatment.
Numbers of Products
Patients' questions
to the pharmacist about common cold symptoms and conditions related to, or
confused with, the cold (e.g., sinus or ear infections, cough, allergy,
influenza) outnumber all other self-care questions combined. Thus, it is vital
for the pharmacist to grasp the complexities of this market. This is not
simple, given the depth and breadth of products marketed in these categories.
Products range from single-entity to combination, with a wide variety of
dosage forms, and include those proven to be effective as well as those of
unknown efficacy and/or safety (e.g., zinc, herbals, homeopathic products).
Single-Entity or
Combination Products
The pharmacist must
first answer the question of whether to recommend several single-entity
products or a combination product. Some basic principles can simplify this
conundrum.
Combination products have
several advantages. The patient needs to purchase only one product, a less
expensive option than buying four separate products. Furthermore, one dose
gives the benefit of two, three, or four ingredients, obviating the need to
dose with four separate products, each potentially with four different dosing
intervals. These products simplify treatment for the patient. Also, the
combination product's integrated label includes instructions,
contraindications, and warnings for all of its ingredients under one heading,
which eases the patient's burden, compared to reading multiple labels.
Finally, patients are gradually becoming more aware and concerned about drug
interactions. The pharmacist can assure these patients that the ingredients of
the combination product do not interact with each other.
Despite the advantages of
combination products, they are void unless one overriding criterion is met by
the product. The patient must have at least one condition that is treatable by
each ingredient. For instance, the patient without any pain or fever should
avoid combination products containing acetaminophen, ibuprofen, or aspirin.
Otherwise, the patient risks experiencing their well-known adverse effects for
no reason. The simple self-care rule to remember is: Any potential risk of
administration must be counterbalanced by a potential benefit.
Single-entity products are the
direct opposite of combination products in every aspect discussed above. It is
generally more expensive to purchase three or four separate products and more
complex to administer them. However, single-entity products do have a large
advantage. If the patient purchases a four-ingredient combination product for
a legitimate use at one time, use of this product may be inappropriate later.
If, with a later illness, he does not have symptoms treatable by all four
ingredients, he cannot alter the product. Unneeded ingredients go along for
the ride. If he purchases the four ingredients as single-entity products, on
the other hand, he is able to tailor therapy to a later condition. For
instance, if he does not have fever or pain, he may administer the ingredients
he does need, omitting internal analgesics. The trade-off in using several
single-entity products is greater expense and increased complexity, contrasted
with an enhanced ability to self-medicate.
The Phenylephrine Controversy
The oral nasal
decongestant market has been relatively stable for a few years since
phenylpropanolamine (PPA) was implicated in causing stroke in a study
initiated by the industry itself. After manufacturers removed PPA, they all
turned to pseudoephedrine as the preferred oral nasal decongestant.3
However, in the past year,
nasal decongestants have undergone another major change. The growing problem
of clandestine methamphetamine labs, and their subsequent toll on Americans,
caused many states to implement strong controls over pseudoephedrine--the major
precursor used to produce methamphetamine. Pseudoephedrine was placed behind
the counter, with new laws mandating that sales be recorded and overseen by a
pharmacist and with strict limits instituted on purchase amounts.
The looming possibility of a
national law to control pseudoephedrine sales drove manufacturers to
substitute phenylephrine for pseudoephedrine in some of their products,
leading to an inconsistent market. For example, some Benadryl, Thera Flu,
Sudafed, and Alka-Seltzer products contain phenylephrine, while others retain
pseudoephedrine. Patients must peruse products carefully to see which
decongestant they contain.
The pharmacist is often asked,
"Which decongestant works better?" or "Which of these lasts longer?" The
latter question is simple to answer. Virtually all phen ylephrine
combinations advise dosing every four hours. On the other hand, several
pseudo ephedrine single-entity and combination products, such as Claritin-D
12 or 24 Hour and Sudafed 12 or 24 Hour, may be dosed less frequently,
increasing the likelihood of compliance. As to comparative efficacy, there is
a dearth of information at this time, as a Medline search will reveal. Both
were approved by the FDA as nasal decongestants years ago. The manufacturers
should supply comparative efficacy data, but many still market both
ingredients, so they are understandably reluctant from a marketing standpoint
to provide such data, since doing so would boost one set of products at the
expense of the other. The pharmacist can advise patients to try both and
choose the one more effective for them. Also, if the patient with nasal
congestion has any contraindications that are shared by both products (e.g.,
difficulty urinating due to an enlarged prostate, heart trouble, diabetes
mellitus, thyroid disease), neither product should be recommended. Rather, the
patient might be urged to try using nasal strips (e.g., Breathe Right).
The congested patient might be
tempted to try SudaCare Shower Soothers, a new product with a prominent
statement on the box that it is from the makers of Sudafed Nasal Decongestant.
The name "Sudafed" could lead the consumer to believe that the product
contains a nasal decongestant, especially due to a phrase on the package:
"Comforting Care When You Are Congested." The product is meant to be placed
onto the floor of the shower when the hot water is running. The front of the
box states that it releases eucalyptus, menthol, and camphor. However, the
ingredients are listed simply as "fragrance." The point is moot, however,
since none of the three ingredients are proven effective for relieving nasal
congestion. Patients who ask the pharmacist about this product should be told
that it does not contain a decongestant.
The FDA's New Sinus
Labeling Rule
In October 2005,
the FDA issued a Final Rule in the Federal Register concerning the role
of nasal decongestants in the treatment of sinusitis.4 For years,
manufacturers have marketed sinus products containing oral nasal
decongestants, usually in combination with analgesics and/or antihis tamines.
The label may have stated that the product was useful for nasal congestion
"associated with sinusitis" or may have included the term "sinusitis." The
agency has concluded that there are no data to support the role of
decongestants (either topical or oral) in the treatment of sinusitis. Data on
their use even as adjunctive therapy are limited and controversial, and
adjunctive use should take place only under the physician's advice.
The FDA considered several
factors in making its decision. First, consumers cannot diagnose or
self-manage sinusitis. Furthermore, evidence shows that use of topical nasal
decongestants negatively affects the resolution of sinusitis and may increase
the degree of sinus inflammation. Also, if patients use decongestants, they
prolong seeking appropriate medical care--a delayed or lost opportunity to
diagnose other serious medical conditions that mimic sinusitis. If asthma and
sinusitis coexist, delaying treatment for either condition could result in
serious complications.
As of
Return of Diphenhydramine
Cough is a
troubling symptom of the common cold.5 Dextro methorphan has been
the major antitussive for nonproductive cough for many years; however, menthol
lozenges, steam inhalants, and chest rubs are also effective. Recent reports
of dextromethorphan abuse may eventually result in stricter controls, similar
to the new laws for pseudoephedrine. Diphenhydramine, an FDA-approved
antitussive for decades, was little seen after several major products were
reformulated. It has returned to the antitussive market and is of little abuse
potential. It is found in Triaminic Thin Strips Grape Flavor, each containing
12.5 mg of diphenhydramine. It is also in several combination products, e.g.,
Sudafed PE Severe Cold Caplets. Pharmacists should warn the patient that
drowsiness may occur and to take care when driving or operating machinery.

REFERENCES
1. Nichol KL,
D'Heilly S, Ehlinger E. Colds and influenza-like illnesses in university
students: impact on health, academic and work performance, and health care
use. Clin Infect Dis. 2005;40:1263-1270.
2. Eccles R.
Understanding the symptoms of the common cold and influenza. Lancet Infect
Dis. 2005;5:718-725.
3. Eccles R, Jawad MS,
Jawad SS, et al. Efficacy and safety of single and multiple doses of
pseudoephedrine in the treatment of nasal congestion associated with common
cold. Am J Rhinol. 2005;
4. Food and Drug
Administration, HHS. Cold, cough, allergy, bronchodilator, and antiasthmatic
drug products for over-the-counter human use: amendment of final monograph for
over-the-counter nasal decongestant drug products. Final rule. Fed Regist
. 2005;70:58974-58977.
5. Chung KF.
Pathophysiology and therapy of chronic cough. Minerva Med.
2005;96:29-40.
6. Caruso TJ, Gwaltney
JM Jr. Treatment of the common cold with echinacea: a structured review.
Clin Infect Dis. 2005;40:807-810.
To comment on this article,
contact
editor@uspharmacist.com.






