US Pharm.
2007;32(9):HS-27-HS-37.
For
many individuals--especially those who are morbidly obese--diet and exercise,
even in combination with drug therapy, are usually not enough to achieve
adequate weight loss.1-4 There is growing consensus that bariatric
surgery is the most effective intervention for achieving sustained weight loss
in the obese population.3-11 In addition, emerging evidence
suggests that bariatric surgery is cost effective from an overall, long-term
health care standpoint, compared with medical management.10,12
However, because of the serious risks associated with it, bariatric surgery is
recommended only for morbidly obese individuals who have not responded to
diet, exercise, and/or medications.1-3 For people with less severe
obesity, the risks of bariatric surgery typically outweigh the potential
benefits.7,13
In the United States, the
number of bariatric surgery procedures has increased significantly over the
past few decades.1,14,15 More than 140,000 people had bariatric
surgery in 2005, compared with approximately 13,000 patients in 1998. This
represents a 1,000% increase between the years 1998 and 2005.3,5
Data suggest that the use of bariatric surgery to control weight is likely to
continue increasing over the next decade.14 For this reason,
pharmacists will be called upon more often to provide services to patients who
have had bariatric surgery.4
Obesity Epidemic
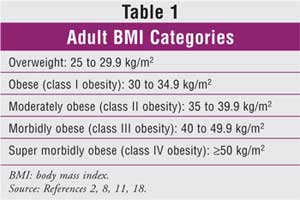
Obesity--defined as
a body mass index (BMI) of greater than 30 kg/m2--is a chronic
medical condition that is increasing in epidemic proportions in the U.S.
3,5,6,8,11,14-20 Table 1 defines obesity classes according to BMI.
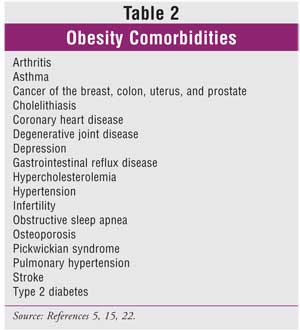
2,8,11,18 Obesity has become a major health problem in the U.S. due to
its high prevalence, causal relationship with serious medical comorbidities (
Table 2), and economic consequences.5,15,21,22 The percentage
of obese American adults increased from 15.3% in 1995 to 23.9% in 2005.16
Today, more than 31% of American adults (~61 million people) are obese.
5,8 Of these, about 4.8% are considered to be morbidly obese.16
Obesity, particularly
abdominal obesity, is associated with an increased risk of type 2 diabetes,
hyperlipidemia, hypertension, obstructive sleep apnea, coronary heart disease,
and stroke.9,11,12,16,17,23 In the U.S., health care expenditures
related to obesity and obesity comorbidities amount to $100 billion annually.
Each year, there are 400,000 deaths attributed to obesity in the U.S.
16,24 The life expectancy of an obese individual is profoundly shorter
than that of a normal-weight individual--for example, a 25-year-old morbidly
obese male has a 22% reduction in expected remaining lifespan, representing an
approximate loss of 12 years of life.17
Clinical Guidelines
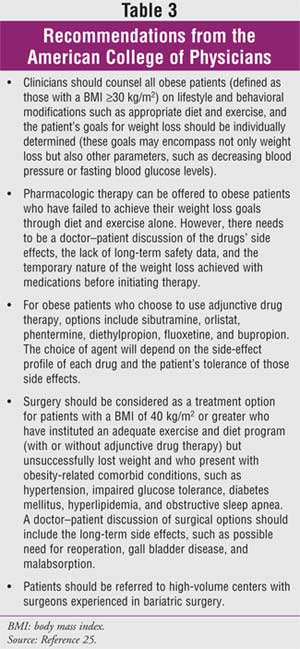
Most clinical
guidelines regarding the role of bariatric surgery have followed the lead of
the 1991 NIH Health Consensus Development Conference by concluding that such
procedures should be considered for patients with either a BMI of greater than
40 kg/m2 or a BMI of greater than 35 kg/m2 with
coexisting medical conditions.6,9,11,14-16 These criteria are
endorsed by the National Heart, Lung, and Blood Institute guidelines for the
treatment of obesity, published in 1998. The criteria are also endorsed in
more recent guidelines published by the Institute for Clinical Systems
Improvement, the American Society for Bariatric Surgery, and the European
Association for Endoscopic Surgery.16 The American College of
Physicians has adopted a somewhat more conservative approach (Table 3),
recommending that bariatric surgery be considered only in patients who have a
BMI of 40 kg/m2 or greater as well as coexisting medical conditions.
16,25,26 In general, each of these guidelines recommends that patients
who are considering bariatric surgery attempt to lose weight prior to surgery,
be free of medical and psychological complications, and be cared for by a
multispecialty team with experience in bariatric surgery and perioperative
care.16
Types of Procedures
Bariatric surgery
procedures can be categorized into operations utilizing one of three methods
to produce weight loss: malabsorptive, restrictive, and mixed technologies.
3,11 Table 4 compares and contrasts the three most commonly used
contemporary bariatric surgery procedures: biliopancreatic diversion, gastric
banding, and gastric bypass.2,3,7-9,11,24
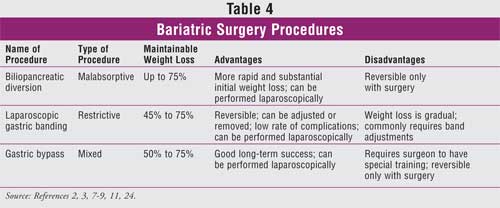
Malabsorptive Procedures:
Malabsorptive procedures decrease the effectiveness of nutrient absorption by
shortening the length of the functional small intestine. Profound weight loss
can be achieved depending on the length of the functional small bowel segment.
However, the benefit of superior weight loss is often offset by significant
metabolic complications, such as protein calorie malnutrition and various
micronutrient deficiencies.8 Although rarely used today,
biliopancreatic diversion with or without duodenal switch is a classic example
of a strictly malabsorptive procedure.7
Biliopancreatic diversion with
or without duodenal switch involves removing part of the stomach.2,7
The remaining section is surgically connected to the lower part of the small
intestine. Weight loss occurs primarily because the contents of the stomach
bypass the majority of the small intestine, thereby passing into the large
intestine before most of the nutrients and calories can be absorbed.7
Inevitable complications associated with this procedure include malabsorption
of carbohydrates, proteins, lipids, minerals, and vitamins. Other
complications include diarrhea, gallstones, hepatic cirrhosis, osteoporosis,
osteomalacia, neuropathy, and night blindness associated with mineral and
vitamin deficiencies. This procedure is rarely performed in the U.S.2
Restrictive Procedures:
Restrictive procedures limit caloric intake by downsizing the stomach's
reservoir capacity. They limit solid food intake by restriction of stomach
size (the only mechanism of action), leaving the absorptive function of the
small intestine intact. Although these procedures are simpler in comparison to
malabsorptive procedures, they tend to produce more gradual weight loss.
Gastric banding is the most commonly performed restrictive procedure.2,8
Gastric banding, which can now
be performed laparoscopically, limits food intake by placing a constricting
ring completely around the top end of the stomach.2 The band is
connected to a narrow tube that extends to an access port just beneath the
skin; a health care provider can narrow or widen the entrance to the stomach
by injection or removal of saline through the port. Passing of food from the
upper pouch to the rest of the stomach is delayed, and the patient feels full
after eating less. Gastric banding is a popular choice of weight-loss surgery,
because it is relatively simple to perform, can be adjusted or removed, and
has a low complication rate. Reported effectiveness of this procedure varies,
with loss of excess weight ranging from 45% to 75% after two years.7
Band-related complications include splenic injury, esophageal injury, wound
infection, band slippage, reservoir deflation/leak, persistent vomiting, and
gastrointestinal reflux disease.2,9,24
Mixed Procedures:
These procedures limit food intake while decreasing absorption of nutrients
within the body.7,8 Gastric bypass, also known as Roux-en-Y
gastric bypass, is the most common mixed surgical procedure used to treat
weight loss in the U.S.7 Gastric bypass combines restriction and
malabsorption techniques, creating both a small gastric pouch and a bypass
that prevents patients from absorbing all they have eaten.2
Roux-en-Y gastric bypass, which has a high success rate, is considered the
gold standard among bariatric procedures. It can be performed as open surgery
or laparoscopically; the laparoscopic procedure is preferred, if possible,
because patients who undergo this procedure typically require less time to
recover and have fewer complications.6,11,27
Approximately 80% of gastric
bypass patients experience a 60% to 80% loss of excess weight in the first
year, with long-term stabilization at 50% to 60% loss of excess body weight
(defined as a BMIof >25 kg/m2 or body weight that exceeds the
ideal BMI).3,28 Generally speaking, weight loss plateaus after one
to two years.7 Complications associated with gastric bypass include
leaks at the junction of the stomach and small intestine, acute gastric
dilation, vomiting, wound hernias, intestinal obstruction, anemia, vitamin and
mineral deficiencies, and dumping syndrome.2
Outcomes of Bariatric
Surgery
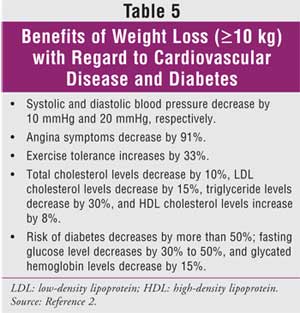
Numerous studies
have demonstrated that bariatric surgery reduces weight up to six times more
than lifestyle modifications and/or diet.13 There are other
advantages to bariatric surgery aside from the dramatic weight loss; published
estimates of the impact of weight loss on cardiovascular disease and diabetes
suggest that substantial benefits are produced by weight loss (Table 5).
2 Data also suggest that compared with controls, patients who underwent
bariatric surgery experienced a significant relative risk reduction of cancer
(76%), endocrine disease (65%), infectious disease (77%), musculoskeletal
problems (59%), nervous system disease (39%), respiratory conditions (76%),
and psychiatric and mental health problems (47%).3
Complications of Bariatric
Procedures
In several
large-scale studies, the mortality rate associated with bariatric surgery was
0.1% to 2%. Common causes of death included pulmonary embolism and serious
surgical complications.15 Identified factors that may increase
mortality include lack of experience by the surgeon, advancing patient age,
male sex, severe obesity (BMI ?50 kg/m2), and coexisting
medical conditions.3,8,16
Common nonfatal perioperative
complications following bariatric surgery include venous thromboembolism,
anastomotic leaks, wound infections, bleeding, incidental splenectomy,
incisional and internal hernias, and early small-bowel obstruction.16
In the only large, well-controlled, prospective study of bariatric
surgery--the Swedish Obese Subjects (SOS) trial--postoperative complications
occurred in 13% of patients. Of these patients, 0.5% experienced bleeding,
0.8% experienced embolism or thrombosis, 1.8% had wound complications, and
6.1% had pulmonary complications.16,29
Rapid weight loss is a known
cause of gallstones. An estimated 30% of patients who have gastric bypass
develop cholelithiasis; routine oral bile salt administration has been shown
to substantially decrease the frequency of this complication. As a result,
most bariatric surgery programs advise bile salt supplementation for the first
six months following gastric bypass.3
Complications from bariatric
surgery may require subsequent readmission or reoperation.16 Data
suggests that 6% to 9% of patients require additional surgeries to correct
complications associated with bariatric surgery. The most common reasons for
the additional surgeries include gastric revision and hernia repair.8
Dumping Syndrome:
Postoperative gastrointestinal complications of bariatric surgery are common.
Nausea and vomiting frequently occur in more than 50% to 70% of patients
undergoing restrictive procedures, partly as a result of eating too much or
eating too rapidly. The dumping syndrome--a complex of neurohormonally mediated
symptoms such as facial flushing, lightheadedness, palpitations, fatigue, and
diarrhea--occurs in more than 50% of patients after Roux-en-Y gastric bypass
when they consume meals high in refined sugars or fats.12,16 The
same phenomenon does not appear to happen after gastric banding procedures.
20 Dumping syndrome may discourage patients from eating foods with a
high sugar content, thus contributing to the beneficial effects of the surgery.
16 Patients who develop dumping syndrome should be advised to avoid
foods that provoke symptoms. Dumping syndrome is rarely severe enough to cause
significant problems with nutritional intake.20
Dietary Considerations
Following Surgery
In the immediate
postoperative period, bariatric surgery patients require a water and
sugar-free, clear-liquid diet. At one day to two weeks, patients can usually
progress to high-protein liquid diets with products such as Boost HP, Ensure
Plus, and Carnation Instant Breakfast. At about two to four weeks following
surgery, most patients can tolerate pureed diets (e.g., yogurt, soups, cottage
cheese, eggs, protein shakes, and soft vegetables). Patients should generally
eat about 3 oz. four to six times per day; drink water and sugar-free, clear
liquids; stop eating if they feel full; and avoid consuming foods and
beverages at the same time (i.e., patients should drink beverages 30 minutes
before or 60 minutes after eating). At around four to six weeks, diets are
usually advanced, including sliced deli meat, cheeses, salads, soups, and
fruits, in addition to the pureed diet. Patients should be encouraged to
slowly add new foods one at a time in small quantities during this transition.
The stomach begins to tolerate larger quantities of food during this period.
Finally, after six weeks, diets should be advanced to include solid foods at
each meal. However, certain foods (e.g., red meats, corn, rice, breads, fruits
with seeds, high-fat foods) often cause vomiting and should be avoided.
Additionally, overeating can cause vomiting and result in electrolyte
imbalances. Clinical dietitians are frequently consulted to recommend
patient-specific diets that maximize calories and prevent dehydration and
electrolyte imbalances.20
Nutritional Deficiencies
Nutritional
deficiencies commonly occur in patients who have undergone bariatric surgery
due to inadequate intake of nutrients and alterations in the digestive anatomy
as a result of surgery.22 It is important to note that nutritional
deficiencies are much more common in patients who have had gastric bypass than
in patients who have had solely restrictive procedures, since restrictive
procedures retain use of the entire gastrointestinal tract.22 Iron
deficiency is the most commonly recognized micronutrient deficiency following
gastric bypass.3 Data suggest that up to 50% of patients suffer
from iron deficiency following gastric bypass.8 Patients also
commonly experience deficiencies in the fat-soluble vitamins (i.e., vitamins
A, D, E, and K).22 Calcium and vitamin D absorption are also
decreased and can lead to hyperparathyroidism. Many patients who have
undergone bariatric surgery experience vitamin B12 deficiency
secondary to decreased intrinsic factor.8 Likewise, thiamine
deficiency has been reported in patients who experience recurrent vomiting.
20
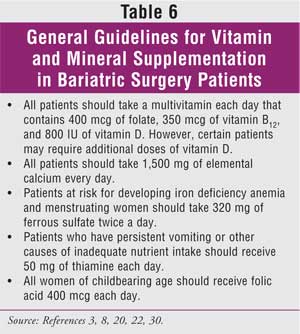
In order to prevent
nutritional deficiencies, bariatric surgery patients require vitamin and
mineral supplements. Table 6 lists general guidelines for administering
these supplements in patients who have had bariatric surgery.3,8,20,22,30
Patients should generally have serum iron, hematocrit, 25-hydroxy-vitamin D,
parathyroid hormone, and vitamin B12 levels monitored at six-month
intervals until stable on replacement therapies; levels should then be
monitored yearly. In addition, bone density should be monitored every one to
two years. Vitamin A should be monitored yearly in all patients who have had
malabsorptive procedures.30
Special Populations
Pregnancy:
Data suggest that weight loss after bariatric surgery may lead to increased
fertility, and this can lead to unwanted pregnancies. Pharmacists should
encourage all sexually active women who have undergone bariatric surgery to
use a backup form of contraception.22 In addition, pharmacists
should inform patients and prescribers that low-dose oral contraceptive
products may have decreased absorption in patients who have had bariatric
surgery.31
Bariatric surgery does not
appear to be associated with adverse perinatal outcomes, and pregnancy after
surgery may be less likely to be complicated by gestational diabetes,
hypertension, and macrosomia.20 The American College of
Obstetricians and Gynecologists (ACOG) recommends that women delay pregnancy
for 12 to 18 months after having bariatric surgery and be evaluated for
nutritional deficiencies. For women who have had gastric banding, the ACOG
recommends that the band be monitored during pregnancy and adjusted
accordingly.20,32
Pediatrics:
Between 1980 and 2002, the prevalence of obesity tripled in children and
adolescents age 6 to 19 years.33 More recent data suggest that one
million adolescents between the age of 12 and 19 years are obese.15
Perhaps more alarming is the fact that obesity-related comorbid diseases are
as prevalent and severe among adolescents as among adults. Specifically,
dramatic increases in the incidence of obesity-related glucose
intolerance/diabetes, metabolic syndrome, premature coronary artery disease
and stroke, and impaired quality of life all indicate that severe obesity
constitutes a major health problem for adolescents and adults. Limited early
experience with bariatric surgery in adolescents suggests that the surgery is
safe and is associated with weight loss, correction of obesity comorbidities,
and improved self-image and socialization.3 However, many experts
feel that adolescent patients may not have proper insight to appreciate the
consequences of undergoing surgery or to cooperate fully with follow-up care.
16
Role of the Pharmacist
It is important for
all pharmacists who take care of patients who have had bariatric surgery to
monitor patient profiles regarding appropriateness of therapy and to have a
basic understanding of bariatric dosing considerations.34 This
knowledge can greatly benefit patients who have had any of the contemporary
procedures.1,4,34
Decreased Medication
Requirements: Many
chronic medical conditions improve quickly during the immediate postoperative
period, necessitating medication changes. Blood pressure, which often
decreases to the normal range without continued therapy, should be monitored
at all postoperative visits. It is important to note that hypotension is
common in the early postoperative period, especially in the presence of
persistent vomiting and poor fluid intake. Patients should be monitored
monthly until blood pressure stabilizes, and antihypertensive medications
should be adjusted accordingly.20
Blood glucose should also be
monitored frequently in the early postoperative period, and patients should be
managed with sliding-scale insulin. Many patients with diabetes have a
decreased need for insulin after bariatric surgery. Discontinuation of all
diabetic medications should be considered when blood glucose normalizes and
after the patient begins to eat.20
Generally, medications for
gastrointestinal reflux should be discontinued after bariatric surgery, since
obesity is one of the primary causes of gastrointestinal reflux. Medications
can be restarted if symptoms recur.20
It is generally ill advised to
decrease or stop psychiatric medications during the immediate postoperative
period. Maintaining patients on psychiatric medications reduces emotional
lability, which is common during the first few months after bariatric surgery.
20
Bariatric Dosing
Considerations: The
reduced size of the stomach after surgery can place patients at risk for
gastrointestinal adverse events; therefore, patients should be instructed to
avoid using nonsteroidal anti-inflammatory drugs and salicylates. Pharmacists
should explain that other options for pain relief exist, including
acetaminophen, opioids, and tramadol. Bisphosphonates should be avoided, since
they too may increase the risk of gastrointestinal ulcerations. Because
patients who have bariatric surgery can be at risk for osteoporosis due to
decreased calcium absorption, other treatment options (e.g., calcitonin nasal
spray, synthetic parathyroid hormone, or raloxifene) should be considered.
Finally, patients should be instructed to avoid oral corticosteroids,
medicinal caffeine, and liquid medications that contain more than 2 g of
sugar, because these too can increase the risk of gastrointestinal problems.
22
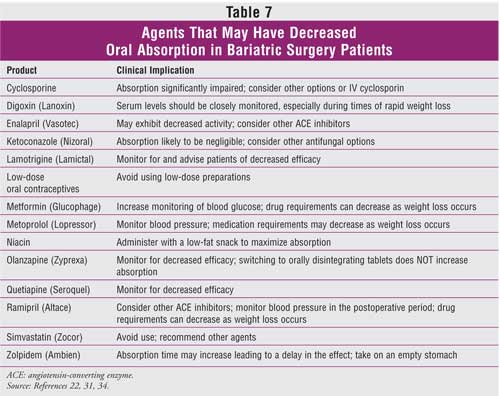
Decreased intestinal length
and surface area in patients who have had gastric bypass can lead to the
reduced absorption of extended-release, delayed-release, and enteric- or
film-coated product formulations. To overcome this problem, the
immediate-release dosage forms should be substituted, which usually requires
increased frequency of administration.22 In addition, drugs that
are rapidly and primarily absorbed in the stomach or duodenum are likely to
exhibit decreased absorption in patients who have had gastric bypass (Table
7).22,31,34
Special considerations also
exist regarding the administration of total parenteral nutrition to patients
who have had bariatric surgery.34 Bariatric surgery patients who
have been receiving nothing orally or who have been on clear liquids prior to
initiation of nutritional support are at an increased risk for developing
refeeding syndrome.35 The syndrome is primarily associated with
hypophosphatemia, as well as declines in serum potassium magnesium and calcium
levels. In rare occurrences, cardiac dysfunction and fluid retention also
occur. The mechanism of these electrolyte abnormalities can be explained by
the acute administration of macronutrients (primarily dextrose) that promote
anabolism (muscle building) in a state of overall depleted electrolyte body
stores (due to postoperative malnourishment). Consequently, carbohydrates and
lipids should generally be dosed lower than the amount needed to maintain
current weight, while protein should be dosed higher in order to avoid muscle
catabolism.34
Conclusion
As the number of
patients undergoing bariatric surgery increases, patient populations who have
had the procedures and present to ambulatory care and hospital pharmacists
will also increase. Accordingly, it is imperative for all clinicians to be
familiar and comfortable with the medication management of these patients.
Clinicians must not only understand the physiologic, metabolic, and
psychological manifestations of morbid obesity but also be cognizant of the
predicted improvement in comorbidities and the potential complications that
can occur in patients who undergo bariatric surgery.20 Clearly,
pharmacists have a vital role, as part of a multidisciplinary team, in
providing bariatric patients with appropriate medical care.34
References
1. Malone M,
Alger-Mayer SA. Medication use patterns after gastric bypass surgery for
weight management. Ann Pharmacother. 2005;39:637-642.
2. Colquitt J, Clegg A,
Loveman E, et al. Surgery for morbid obesity. Cochrane Database Syst Rev
. 2005;4:CD003641.
3. Elder KA, Wolfe BM.
Bariatric surgery: a review of procedures and outcomes. Gastroenterology
. 2007;132:2253-2271.
4. Malone M. Enhancing
pharmacist involvement in weight management--time to get with the program.
Ann Pharmacother. 2004;38:1961-1963.
5. Markel TA, Mattar
SG. Management of gastrointestinal disorders in the bariatric patient. Med
Clin North Am. 2007;91:443-450, xi.
6. Hutter MM, Randall
S, Khuri SF, et al. Laparoscopic versus open gastric bypass for morbid
obesity: a multicenter, prospective, risk-adjusted analysis from the National
Surgical Quality Improvement Program. Ann Surg. 2006;243:657-662,
discussion 662-666.
7. Sanchez VM,
Schneider BE, Mun EC. Patient information: Weight loss surgery. In: Rose BD,
ed. UpToDate. Waltham, MA; 2007
8. Sanchez VM,
Schneider BE, Mun EC. Complications of bariatric surgery. In: Rose BD, ed.
UpToDate. Waltham, MA; 2007.
9. Obesity. In: Feldman
M, Tschumy WO, Friedman LS, Sleisenger MH, eds. Sleisenger and Fordtran's,
Gastrointestinal, and Liver Disease. 7th ed. Philadelphia, PA: Elsevier;
2002:321-332.
10. Poulose BK, Holzman
MD, Zhu Y, et al. National variations in morbid obesity and bariatric surgery
use. J Am Coll Surg. 2005;201:77-84.
11. Sanchez VM,
Schneider BE, Mun EC. Surgical management of severe obesity. In: Rose BD, ed.
UpToDate. Waltham, MA; 2007.
12. Wadden TA, Sarwer
DB, Fabricatore AN, et al. Psychological and behavioral status of patients
undergoing bariatric surgery: what to expect before and after surgery. Med
Clin North Am. 2007;91:451-469, xi-xii.
13. Mitka M. Surgery
useful for morbid obesity, but safety and efficacy questions linger. JAMA
. 2006;296:1575-1577.
14. Kuruba R, Koche LS,
Murr MM. Preoperative assessment and perioperative care of patients undergoing
bariatric surgery. Med Clin North Am. 2007;91:339-351, ix.
15. Rendon SE, Pories
WJ. Quality assurance in bariatric surgery. Surg Clin North Am.
2005;85:757-771, vi-vii.
16. DeMaria EJ.
Bariatric surgery for morbid obesity. N Engl J Med. 2007;356:2176-2183.
17. Buchwald H, Avidor
Y, Braunwald E, et al. Bariatric surgery: a systematic review and
meta-analysis. JAMA. 2004;292:1724-1737.
18. Powers KA, Rehrig
ST, Jones DB. Financial impact of obesity and bariatric surgery. Med Clin
North Am. 2007;91:321-338, ix.
19. McNatt SS, Longhi
JJ, Goldman CD, McFadden DW. Surgery for obesity: a review of the current
state of the art and future directions. J Gastrointest Surg.
2007;11:377-397.
20. Boan J. Management
of patients after bariatric surgery. In: Rose BD, ed. UpToDate.
Waltham, MA; 2007.
21. AGA guidelines:
obesity. Gastroenterology. 2002;123:879-881.
22. Miller AD, Smith
KM. Medication and nutrient administration considerations after bariatric
surgery. Am J Health Syst Pharm. 2006;63:1852-1857.
23. McDermott AY.
Conference coverage: selected presentations from the 20th Annual Practical
Approaches to the Treatment of Obesity. Medscape General Medicine.
2006;8(4):61.
24. Korenkov M,
Sauerland S, Junginger T. Surgery for obesity. Curr Opin in Gastroenterol
. 2005;21:679-683.
25. Snow V, Barry P,
Fitterman N, et al. Pharmacologic and surgical management of obesity in
primary care: a clinical practice guideline from the American College of
Physicians. Ann Intern Med. 2005;142:525-531.
26. Stanton M. American
College of Physicians offers drug and surgery recommendations for obesity.
DOC News. American Diabetes Association; 2005.
27. Lee WJ, Yu PJ, Wang
W, et al. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment
of morbid obesity: a prospective randomized controlled clinical trial. Ann
Surg. 2005;242:20-28.
28. Obesity. In:
Feldman M, Tschumy WO, Friedman LS, Sleisenger MH, eds. Sleisenger and
Fordtran's Gastrointestinal and Liver Disease. 7th ed. Philadelphia,
PA: Elsevier; 2002:321-332.
29. Sjöström L,
Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk
factors 10 years after bariatric surgery. N Engl J Med.
2004;351:2683-2693.
30. Mason ME, Jalagani
H, Vinik AI. Metabolic complications of bariatric surgery: diagnosis and
management of issues. Gastroenterol Clin North Am. 2005;34:25-33.
31. Malone M. Altered
drug disposition in obesity and after bariatric surgery. Nutr Clin Pract
. 2003;18:131-135.
32. ACOG Committee
Opinion #315: obesity in pregnancy. Obstet Gynecol. 2005;106:671.
33. Ogden CL, Carrol
MD, Curtin LR, et al. Prevalence of overweight and obesity in the United
States, 1999-2004. JAMA. 2006;295:1549-1555.
34. Fussy SA. The
skinny of gastric bypass. US Pharm. 2005;30(2):HS3-HS12.
35. Farraye FA, Forse
A. Nutritional consequences following bariatric surgery. In: Anderson WA,
Foresta L, eds. Bariatric Surgery: A Primer for Your Medical Practice.
Thorofare, NJ: Slack, Inc.; 2005. Chapter 8.
To comment on this article, contact
editor@uspharmacist.com.





