US Pharm.
2008;33(1):50-52.
Dystonia is a term used to
describe a neurologic movement disorder characterized by prolonged involuntary
muscle contractions resulting in repetitive twisting motions and abnormal
postures of the neck or torso.1,2 Contractions may affect a single
group of muscles in the neck or torso, but adjacent muscle groups may also be
affected.3 Dystonia is often difficult to diagnosis because it can
be confused with spasticity or rigidity, leading to misdiagnoses such as
cervical muscle strain in adults and cerebral palsy in children.3
The exact cause of dystonia is unknown,Ü but experts believe that those
suffering from dystonia lack the ability to properly process neurotransmitters
in the brain. Some of the neurotransmitters involved in muscle contractions
are gamma-aminobutyric acid (GABA), dopamine, acetylcholine, norepinephrine,
and serotonin.2 It is also thought that dystonia may be caused by
environmental factors or result from an injury to the basal ganglia of the
brain. The symptoms of dystonia initially are often mild, but as time
progresses they become more noticeable. Symptoms have been documented with
heavy-metal poisonings, trauma, and adverse reactions to medications.2
Dystonia is classified
according to the area of the body that is affected. Generalized dystonia
affects most parts of the body; focal dystonia affects one specific area of
the body; multifocal dystonia affects more than one unrelated area of the
body; segmental dystonia affects more than one adjacent part of the body; and
hemidystonia involves the limbs of one side of the body.2,4 The
most common type of dystonia is focal dystonia, with cervical dystonia (CD) or
spasmodic torticollis being the most prevalent.5
Etiology
Cervical dystonia
is the third most common movement disorder after Parkinson's disease and
tremor.6 Approximately 90,000 people in the United States are
living with CD.3 The most common form of CD is torticollis, which
is the rotation of the neck to one side.5 Cervical dystonia is
characterized by a syndrome of sustained or intermittent involuntary
contractions of the neck muscles and abnormal head postures, and it is
frequently associated with pain.5 The exact etiology of CD is
unknown; it may result from stroke, cervical cord injuries, trauma to the head
or neck, or genetic predisposition, or it may be induced by certain
medications such as levodopa or neuroleptics.6,7 The predominant
risk factors include female gender (twice as likely to occur in women as men),
age (most likely to occur between the ages of 30 and 70), and a history of
head or neck injury (5%ñ16% occurrence).6 Symptoms include the
involuntary turning, tilting, or extension of the neck muscles, as well as
tremor, pain, and stiffness or tightness of the neck.6 This
condition may lead to physical disabilities and adversely affect the patient's
quality of life. There is no cure for CD; it is primarily managed
through pharmacotherapy and, in rare instances, surgical denervation.6
Treatment
Pharmacotherapy for
cervical dystonia has historically included anticholinergics, skeletal muscle
relaxants, benzodiazepines, and tricyclic antidepressants.8,9
Unfortunately, use of these agents has been limited due to their undesirable
adverse effects. Anticholinergic medications such as trihexyphenidyl and
benztropine have shown some success in CD, usually at higher doses. Their
pharmacologic effects are achieved by blocking acetylcholine. This same
mechanism is responsible for the following adverse effects that make these
medications difficult to tolerate: confusion, drowsiness, amnesia,
constipation, xerostomia, and urinary retention.10-12 Skeletal
muscle relaxants such as baclofen were often used in treating CD due to their
ability to calm muscle spasticity.9,10 Baclofen is a derivative of
GABA and is thought to act at the level of the spinal cord to cause muscle
relaxation.11,13 Drowsiness is the most common adverse effect,Ü
while confusion, dizziness, and nausea may also occur. Benzodiazepines such as
clonazepam, lorazepam, and diazepam augment the inhibitory effects of GABA,
which leads to their skeletal muscleñrelaxant properties and utility in CD.
9,10 It is possible for patients to tolerate high doses of
benzodiazepines, but common and often dose-limiting adverse effects include
sedation, confusion, dizziness, ataxia, and headache.11 Tricyclic
antidepressants as well as carbamazepine (structurally related to the
tricyclic antidepressants) have been used for CD in the past.9 The
ability of these agents to block acetylcholine is the most likely explanation
for their function in CD as well as for their limited use in this condition.
Common adverse reactions include sedation, confusion, dizziness, and
constipation.11,13
In 1989, the FDA approved the
use of botulinum toxin type A (BoNTA) for the treatment of blepharospasm, a
focal dystonia affecting the eye.10 In 2000, the FDA approved the
use of BoNTA (Botox) and botulinum toxin type B (BoNTB as Myobloc) for the
treatment of CD.10 Chemodenervation with botulinum toxin is the
most effective treatment for CD, with more than 80% of those afflicted
achieving relief of symptoms.8 BoNTA is considered the first-line
therapy for CD, and BoNTB is considered an alternative for those nonresponsive
to type A.10,14,15
Botulinum toxin is the most
neurotoxic substance known to man.16 It is produced by the
bacterium Clostridium botulinum and has seven different serotypes (A,
B, C, D, E, F, and G).10,14 Each serotype has distinctively
different properties and actions with an affinity to different proteins. BoNTA
cleaves the synaptosomal-associated protein of 25 kd or SNAP-25, and BoNTB
cleaves synaptobrevin.8,14 All botulinum serotypes work at the
presynaptic nerve terminals, preventing the release of acetylcholine. The lack
of acetylcholine results in the denervation of the muscle, producing paralysis.
14 Doses for BoNTA and BoNTB are not equivalent. Botulinum toxin type A
is commercially available in 100-unit vials and botulinum toxin type B is
commercially available in 2,500-, 5,000-, and 10,000-unit vials.5,8,14-16
The use of botulinum toxin is generally well tolerated. The most common
adverse effects are dysphagia (approximately 20% of patients), upper
respiratory infection, dry mouth, dyspepsia, and injection site pain.
5,15-17
Treating CD with botulinum may
require a trial phase to determine the exact dose needed and the specific
injection sites to alleviate symptoms.10 Botulinum toxin injections
should only be injected into the muscles responsible for the abnormal posture.
High doses (e.g., greater than 400 units of type A) or frequent injections
(less than three months apart) should be avoided.17,18 BoNTA is the
most studied serotype for the treatment of CD. According to a Cochrane review,
eight studies have compared BoNTA to placebo, proving it is a safe and
effective drug for the treatment of CD.18 However, concerns about
long-term treatments and the development of immunoresistance may limit its
usefulness in those who become unresponsive to BoNTA.17,18 Three
studies have compared BoNTB to placebo to test its safety and efficacy in the
treatment of CD.19 Both reviews concluded that both BoNTA and BoNTB
are safe and effective treatments. Only two studies have directly compared
BoNTA and BoNTB to each other. Comella et al compared the clinical efficacy of
BoNTA versus BoNTB in CD, and Tintner et al directly compared the autonomic
effects of both serotypes.8,20 These studies concluded that BoNTA
had a longer duration of action than BoNTB, but patients experienced more
constipation and less saliva production with BoNTA than with BoNTB. Other
autonomic symptoms were similar between the serotypes.17,20 BoNTB
is a viable option for those patients who have developed resistance to BoNTA.
According to the American Academy of Neurology, physicians need to be
specially trained in the pharmacology and proper clinical use of botulinum
toxin; those untrained should not administer it.17 Injections are
individualized, and modifications to a treatment regimen must be based on
prior responses.17 It is recommended that physicians attend at
least one course to acquire the necessary skills and gain experience to be
competent in the administration of botulinum toxin injections for CD.17
Botulinum toxin injections can be administered on an outpatient basis with the
use of electromyography (EMG).17 EMG produces a sound that can
identify the electrical activity of the muscle while at rest and when it
contracts. This tool is useful to ascertain which muscles require injections
when they are not easily identified through physical examination.17
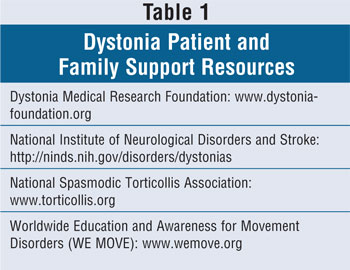
The Dystonia Medical Research Foundation and other support agencies are
available to find physicians adequately trained in movement disorders and in
the administration of botulinum toxin injections (TABLE 1).
Nonpharmacologic or
complementary treatments have been used in conjunction with pharmacologic
therapies to maximize results. Complementary treatments included physical
therapy to stretch and strengthen muscles, relaxation techniques or
stress-reduction activities, yoga, and acupuncture.3,10
Surgery
Surgical removal of the nerves
responsible for the overactive muscles have been performed with focal
dystonias such as CD, but these surgeries have had inconsistent results with
short-term relief of symptoms.2,3 Deep brain stimulation of the
globus pallidus is reserved for those patients refractory to current
pharmacologic treatments.3,10 Electrodes are implanted in targeted
areas of the brain and a battery-operated pulse generator is implanted under
the patient's skin in the intraclavicular area. The electrodes and the
generator are connected by a thin wire extending from a small opening in the
skull to the generator under the collarbone.3,10,17 Implantation of
the generator is performed under anesthesia, but the patient is awake during
implantation of the electrodes to aid the surgeon in monitoring the patient's
brain function.10 The batteries in the generator are activated and
electrical currents are sent to the brain. Voltage settings are individualized
and may take months to adjust to the correct voltage. This surgery does not
eliminate the possible need for further pharmacologic treatments such as
botulinum toxin injections.10 As with any surgery, risks include
hemorrhage (rare), infection, and hardware malfunctions.10
Summary and Conclusion
Cervical dystonia
is the third most common movement disorder. Currently, there is no cure for
CD, but treatment options have improved over the years to enhance the quality
of life for those suffering from this condition. Botulinum toxins type A and
type B have been available for patients with CD since 2000. This therapy is
more advantageous than past pharmacotherapeutic options for CD, which were
limited in use due to significant adverse reactions. Botulinum toxins have
resulted in modest effects by providing symptomatic relief and improving
overall quality of life. The National Institute of Neurological Disorders and
Stroke is currently conducting research to possibly find a cure and better
treat those who are afflicted with dystonia.
References
1. Fahn S, Marsden CD, Calne DB. Classification and investigation of dystonia. In: Marsden CD, Fahn S, eds. Movement Disorders 2. London, England: Butterworths; 1987:332-358.
2. Dystonias Fact Sheet. National Institute of Neurological Disorders and Stroke. Available at: http://ninds.nih.gov/disorders/dystonias/details_dystonias.htm. Accessed October 15, 2007.
3. Tarsy D, Simon D. Dystonia. N Engl J Med. 2006;355:818-29.
4. Fahn S, Bressman SB, Marsden CD. Classification of dystonia. Adv Neurol. 1998;78:1-10.
5. Botulinum toxin for cervical dystonia. Med Lett Drugs Ther. 2001;43:63-64.
6. Jankovic J, Leder S, Warner D, Schwartz K. Cervical dystonia: clinical findings and associated movement disorders. Neurology. 1991;41:1088-1091.
7. Frei K, Pathak M, Jenkins S, Truong D. Natural history of posttraumatic cervical dystonia. Move Disord . 2004;12:1492-1498.
8. Comella C, Jankovic J, Shannon K, et al. Comparison of botulinum toxin serotypes A and B for the treatment of cervical dystonia. Neurology. 2005;65:1423-1429.
9. Greene P, Shale H, Fahn S. Analysis of open-label trials in torsion dystonia using high dosages of anticholinergics and other drugs. Mov Disord. 1988;3:46-60.
10. Dystonia Medical Research Foundation. Available at: www.dystonia-foundation.org. Accessed October 5, 2007.
11. Clinical Pharmacology Web site. Available at: http://cp3.clinicalpharmacology-ip.com. ezproxy. mcphs.edu. Accessed October 30, 2007.
12. Burke RE, Fahn S, Marsden CD. Torsion dystonia: a double-blind, prospective trial of high-dosage trihexyphenidyl. Neurology. 1986;36:160-164.
13. Micromedex Healthcare Series Web site. Available at: www.thomsonhc.com/ezproxy.mcphs.edu/home/dispatch. Accessed October 30, 2007.
14. Berman B, Seeberger L, Kumar R. Long-term safety, efficacy, dosing and development of resistance with botulinum toxin type B in cervical dystonia. Move Disord. 2005; 20:233-237.
15. Botox [package insert]. Irvine, CA: Allergan, Inc.
16. Myobloc [package insert]. Malvern, PA: Solstice Neuroscience, Inc.
17. Comella C, Janovic J, Mitchell B. Use of botulinum toxin type A in the treatment of cervical dystonia. Neurology. 2000;55(suppl 5):S15-S21.
18. Costa J, Espirito-Santo C, Borges A, et al. Botulinum toxin type A therapy for cervical dystonia. Cochrane Database of Systematic Reviews. 2. 2006.
19. Costa J, Espirito-Santo C, Borges A, et al. Botulinum toxin type B for cervical dystonia. Cochrane Database of Systematic Reviews. 1. 2006.
20. Tintner R, Gross R, Winzer U, et
al. Autonomic function after botulinum toxin type A or B: a double-blind,
randomized trial. Neurology. 2005;65:765-767.
To comment on this article, contact
edito@uspharmacist.com.






