US Pharm. 2006;8:96-102.
Erectile dysfunction (ED) is a common health problem. It is estimated that the incidence of ED among men at age 50 is approximately 50%, and at age 70 it may be as high as 70%.1-3 Many men find it difficult to discuss their sexual health with their health care providers and avoid the subject altogether. Some men feel that sexual performance is an indicator of masculinity and virility and that admitting that they have a problem with sexual performance diminishes their manliness. Many men who have ED do not understand that the condition may be caused by an underlying problem such as a disease state or medication. If the cause can be identified and treated, the ED may improve. Also, there are several effective treatment options for ED that might enhance sexual performance. Therefore, it is imperative that pharmacists and other health care providers engage patients in a dialogue concerning their sexual health. It is critical that the pharmacist be empathic, caring, and sensitive.
Unfortunately, many practitioners feel equally uncomfortable discussing this sensitive subject with their patients. If you are nodding your head because you often skirt around these topics when interacting with patients, hopefully, this article will help. The goal of this article is to provide guidance on how to discuss sensitive issues concerning men's sexual health with your patients.
First, let's consider a few basics. It is important to remember that ED is a complex disease state, because it can significantly impact a person's sense of worth, self-confidence, quality of life, and intimate relationships.2 When counseling the patient with ED, it is important for the pharmacist to realize that he or she is treating the whole person, not just one part of the patient's anatomy. While ED may be effectively treated by drug therapy, the ability to achieve an erection is not synonymous with intimacy and does not necessarily solve all of a man's problems. Patients might not have had intercourse for a long time. Reestablishing intimacy between partners can often be uncomfortable or difficult, and the couple might require counseling to heal their relationship.
Men who have ED often experience a multitude of emotions, including embarrassment, shame, isolation, and inadequacy, all of which are barriers to communication. They often have difficulty talking about the problem with anyone, even their partner. A man may feel that he is the only one experiencing these sensitive challenges. Only a small percentage of patients will initiate a dialogue with their health care provider. Due to the sensitive nature of this topic, it is important to realize that counseling about drug therapy is only one issue that needs to be addressed. Therefore, it is essential that the pharmacist appear relaxed, open, and nonjudgmental in discussing ED and related issues.
Pharmacists must examine their own reactions and do whatever possible to become comfortable initiating a discussion with patients and partners affected by ED. For instance, displaying anxiety while talking about ED with a patient will cause a conversation to be unproductive. When people become anxious, they usually have a fairly stable, patterned response. Some avoid conversations--they withdraw. Some try to fix things--they try to "make it better," for example, by saying, "Don't worry, it will be all right." Others try to minimize the problem by telling the patient, "It's not the end of the world," or "Gee, there are certainly worse problems to have." None of these responses show empathy or help the patient with ED. The problem needs to be taken seriously and discussed calmly and openly. Pharmacists can learn to use their anxiety as a stimulus to listen more carefully and reflect back understanding.
The Patient Interview
To set a relaxed
and comfortable stage for open communication, pharmacists must be clinically
well prepared to evaluate the condition and provide patient education on the
topic. It is important to be professional, confident, and caring when engaging
patients. A lack of confidence can be misunderstood by the patient. If a
pharmacist hesitates, flushes, stutters, loses eye contact, or sounds unsure
about what to ask or say next, he or she might send the wrong signal to the
patient. The patient might think that the pharmacist is surprised or
embarrassed by the topic or that he or she is being judgmental. Thus, the
pharmacist should develop an organized approach to a patient interview.
First, be sure to define the problem. ED is the inability to obtain and maintain an erection firm enough for sexual intercourse.2 Male sexual dysfunction might also include problems with libido, anatomical abnormalities, and/or ejaculatory dysfunction. 2,3 Medications intended to treat ED might not address all of the symptoms a patient is experiencing. If a patient is experiencing decreased libido, he should be referred to a physician for endocrinology testing (e.g., testosterone levels, thyroid function).2,3 If the patient has problems with intimacy, he might benefit from psychological counseling. If a patient has an anatomical problem, such as a curved penis, he needs to have a physical examination.3 Therefore, it is important to explore precisely what the patient is experiencing by asking specific questions. Also, understanding the patient's pattern of symptoms allows the pharmacist to ascertain the patient's expectations from pharmacotherapy. The pharmacist can evaluate whether the patient's expectations are realistic. Not all patients who experience a decrease in sexual satisfaction have ED. For instance, a man might be able to achieve an erection sufficient for vaginal penetration and climax, but he might not be satisfied with its firmness, possibly seeking a better erection reminiscent of youth. These expectations may not be realistic given his age and level of health.2,3
The pharmacist should develop a list of questions that will enable him or her to assess the problem with confidence, authority, and professionalism. For example, the pharmacist might ask a male patient:
• Do you experience sexual
desire?
• Do you want to
engage in sexual intercourse?
• Are you
experiencing intimacy problems with your partner?
• Do you
have difficulty achieving and maintaining erections?
• How often do
you achieve an erection?
• Do you
experience erections during sleep, while dreaming, or in the mornings?
• Are your
erections firm enough to achieve penetration?
• Do you
have problems reaching a climax?
• Do you
have problems ejaculating?
• Do you
experience anxiety when thinking about intercourse?
• Are there
times when your ED is worse? If so, in which situations?
• Are you
experiencing any depression?
• Do you feel
sad, blue, or "down in the dumps"?
• Have you
noticed a decreased pleasure in life?
• Are you
happy with your sexual partner?
• Do you
have a good relationship with your sexual partner?
• When did
this problem begin? Was it abrupt or gradual?
• How has ED
affected your sex life?
• Are you or
your partner angry about this problem?
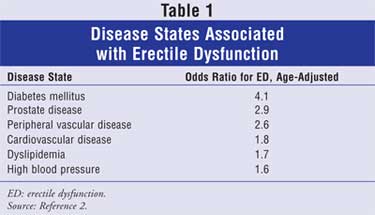
Next, the pharmacist should screen for any known causes of ED. ED can be a warning sign that the patient has an underlying health problem. The pharmacist should ask a number of questions to screen for diabetes or cardiovascular disease. If the equipment is available, the pharmacist can check the patient's vital signs and blood glucose and lipid levels.2,3 There is some indication that ED may be associated with prostate problems, so it is important to screen for any genitourinary health issues.2 Also, it is important to collect a complete social history, including information on tobacco and alcohol use, as well as exercise habits, since many substances and activities can interfere with sexual function.2,3 A list of disease states that increase the risk of ED can be found in Table 1.2 The most common organic causes of ED are vascular disease (40%) and diabetes (30%).2 If a patient has a risk factor, sign, or symptom of any of these conditions, the pharmacist should refer him to his health care provider for further evaluation and management. The patient should be aware that ED might be an indicator of other health problems. To screen for these conditions, ask the following questions:
• Have you ever been
diagnosed with diabetes, high blood pressure, or high cholesterol?
• Are you
experiencing any changes in your appetite, thirst, urinary patterns, or
weight?
• Do you
have any history of disease involving the heart, blood vessels, nerves, or
hormones?
• Have you
ever had urogenital trauma or surgery?
• Have you ever
been diagnosed with prostate problems?
• Do you
experience any problems with urinary voiding? Do you experience urgency,
frequency, straining, hesitancy, incomplete bladder emptying, or weak urine
stream?
• Do you
smoke or use any tobacco products?
• Do you
drink alcohol?
• Do you use
recreational drugs such as marijuana, cocaine, or heroin?
• How active
are you throughout the day? Do you engage in regular aerobic exercise?
• What are
your hobbies? Do you routinely ride bicycles, motorcycles, or horses? Do you
take regular cycling classes at the gym?
The pharmacist should also screen for possible drug-induced disease. Some medications have a direct impact on the physiological changes that occur during arousal and result in an erection. Medications that are highly anticholinergic decrease parasympathetic activity, resulting in ED. For instance, first-generation antihistamines, tricyclic antidepressants, phenothiazines, or antiparkinson drugs may increase the risk of ED. Other medications interfere with erections by lowering blood pressure and therefore the pressure gradient in the pelvic region. Although any medication used to treat hypertension can cause this problem, diuretics, peripheral beta-blockers, and central sympatholytics are the most common culprits. Angiotensin-converting enzyme inhibitors, calcium channel blockers, and alpha-blockers have not demonstrated the same risk. Other med-ications alter the patient's response to sexual stimulation either directly or indirectly. Central nervous system depressants, such as alcohol, narcotics, benzodiazepines, and barbiturates, may blunt the patient's sexual arousal. Other medications such as dopamine agonists, estrogens, and antiandrogens interfere with the production of testosterone in the body.2-7 This results in a drop in libido.4-7
Approaching the Patient
The pharmacist
might interface with a patient who is experiencing ED at different stages of
the diagnosis and management of the disorder. For instance, the pharmacist
might initiate a discussion with the patient upon noting that the patient has
a medical condition that increases the risk of ED. As the patient might not
have been aware that his other health conditions may cause problems with
sexual satisfaction, he may begin to adhere more closely to his health care
provider's recommendations concerning lifestyle and medications. The
pharmacist can help by recommending interventions to improve the patient's
overall health and by reinforcing the importance of medication compliance to
optimize blood glucose and blood pressure control.
The pharmacist has another opportunity to engage the patient when he picks up medication refills. The pharmacist might note that the patient is taking a drug that increases the risk of ED; he or she might then discuss urogenital health with the patient. For instance, the pharmacist might note that the patient has been taking medication for blood pressure control. The pharmacist might say, "I notice that you have been taking propranolol now for three months. One possible side effect of this medication is erectile dysfunction (or having trouble achieving an erection). Have you noticed any change in your sexual performance since initiating this medication? If so, we can talk to your doctor about recommending an alternative medication that has a decreased risk of this effect." This pharmacist-initiated conversation offers the patient a safe environment to talk about ED. The patient is now aware that this is a common problem that is acceptable to discuss. It provides an opportunity for the patient to share his thoughts, experiences, and concerns.
Finally, the pharmacist might
interface with the patient when he presents with a new prescription for ED
treatment (e.g., a phosphodiesterase type 5 inhibitor). When dispensing a new
prescription for an ED treatment, it is important to talk to the patient and
explore his questions, concerns, and expectations. Remember, because patients
with ED do not often initiate discussions about their problem, pharmacists may
need to start the conversation--even for those with a prescription. Some
suggestions for initiating
a conversation
include the following questions and comments:
• I would like to talk to
you about your new prescription to ensure that it will be effective for you. I
know that this may not be easy to discuss, but I would like to answer any
questions you or your partner may have.
• What has
your doctor already told you about erectile dysfunction and how this medicine
will help?
• Has your
physician suggested counseling?
• What
questions do you have, now that you have a prescription to treat erectile
dysfunction?
• I am going to
tell you what you need to know about this medicine. If you have any questions,
please ask. I want you to be as informed as possible.
While it may not be within the pharmacist's role or training to discuss intimacy, it certainly would be appropriate to ask if the couple would like a referral to a counselor. A therapist can counsel the couple about fears and anxieties regarding ED and reestablishing intimacy. The pharmacist can address fears about the medication, what it can or cannot accomplish, and what side effects are possible.
Conclusion
Even though ED can
be a sensitive and uncomfortable topic for the patient and health care
provider, pharmacists need to discuss ED in a way that is comfortable for all
involved. By using the steps discussed in this article, the pharmacist can
provide better care to patients with ED and their partners.
REFERENCES
1. Feldman HA,
Goldstein I, Hatzichristou DG, et al. Impotence and its medical and
psychosocial correlates: results of the Massachusetts Male Aging Study. J
Urol. 1994;151:54-61.
2. Burnett AL. Erectile
dysfunction. J Urol. 2006;175:S25-S31.
3
. Beckman TJ, Abu-Lebdeh HS, Mynderse LA. Evaluation and medical management of
erectile dysfunction. Mayo Clin Proc. 2006;81:385-390.
4. Kochar MS, Mazur LI,
Patel A. What is causing your patient's sexual dysfunction? Uncovering a
connection with hypertension and antihypertensive therapy. Postgrad Med
. 1999;106:149-157.
5. Lee M. Erectile
dysfunction. In: DiPiro JT, Matzke GR, Posey LM, et al, eds.
Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw-Hill;
2005:1515-1533.
6. Klasco RK, ed.
DISEASEDEX System. Greenwood Village, Colo: Thomson Micromedex (Edition
expires [06/2006]).
7. Thompson JF.
Geriatric urologic disorders. In: Alldredge BK, Corelli RL, Guglielmo BJ, et
al. Applied Therapeutics: The Therapeutic Use of Drugs. Baltimore:
Lippincott Williams & Wilkins; 2005:101-1–101-33.
To comment on this article, contact editor@uspharmacist.com.






