US Pharm. 2006;7:16-22.
Croup causes substantial
morbidity, especially during flu seasons. The characteristic barking cough it
produces can be extremely troubling to parents, as they often think their
child is seriously ill. Fortunately, most cases of croup are mild and are
treatable with simple self-care measures such as vapor therapy.
Croup is a community-acquired
infection that results in inflammation of the larynx, bronchi, and trachea. In
children, it is usually sufficiently mild for outpatient treatment, but the
less common form seen in adults may require hospitalization.1,2
Croup occurs in as many as 6% of children ages 6 months to 6 years.3
Etiology
Croup may be due to
such bacteria as Mycoplasma pneumoniae, Corynebacterium diphtheriae,
or Streptococcus pneumoniae.1 However, viral invaders are
most often responsible for pediatric croup, also known as laryngotracheobronchitis.4
Parainfluenza causes more than 66% of cases, and the particular variant caused
by human parainfluenza virus 1 has the peculiar phenomenon of occurring since
1973 in odd-numbered years.1,2,4,5 Clinicians also observe a
clustering of croup cases corresponding to outbreaks of influenza A and B.1,4,5
Croup resulting from influenza A is less common but more severe than croup
arising from parainfluenza or respiratory syncytial virus.5 Other
viruses that may cause croup include metapneumovirus, adenovirus, rhinovirus,
enterovirus, measles virus, and herpes simplex virus.4 Patients
usually contract these viruses via the standard mechanisms by which
aerosolized viral illnesses are contracted (e.g., direct inhalation,
contamination of the hands followed by touching the mucosa of the eyes, nose,
or mouth).1 The incubation period is two to six days.4
Following inoculation, the progression of the viral invaders is to the nasal
mucosa and trachea. Airways are narrowed by inflammation of the larynx,
trachea, and bronchi, as well as by heightened production of mucus.
Epidemiology
Croup is most
common in children ages 6 months to 3 years, although it can be seen up to age
15 years and occasionally in adults.1,4,6,7 Viral croup is more
common in males, with a male–female ratio of 3:2.4,6 The peak
age for viral croup is 2 years.2 Most cases arise in the winter or
fall.6 If one member of a family has croup, the risk of passing it
to other members of the household is 15%.6
Manifestations of Croup
Patients undergo a
prodrome of two- to four-day duration in which they perceive the onset of a
respiratory infection in the upper airways, manifested by rhinorrhea, mild
cough, and low-grade fever.4 Eventually, release of inflammatory
factors causes erythema, exudate, and inflammation, culminating in symptoms
such as cough. The cough of croup is a harsh barking, resembling the sound
made by a seal.1,8 The cough may produce hoarseness from swelling
of the vocal cords.4,9 Swallowing is usually unaffected. Croup
often worsens at night, leading to many visits to emergency departments and
late-night calls to family physicians.8
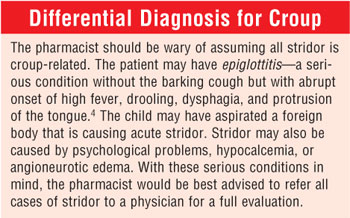
Croup is the most common cause
of nonchronic pediatric stridor.6 Stridor on inspiration coexisting
with coarse rhonchi is caused by a turbulent airflow arising from respiratory
obstruction.10 The patient may suffer shortness of breath,
tachycardia, or tachypnea.7 Nostrils may flare. Babies and young
children may exhibit supraclavicular, infraclavicular, intercostal, and
sternal retractions, where the chest and stomach muscles appear to suck in
with each breath.4,8 Rhinorrhea may also be present, but fever is
absent or mild. The child may be unable to rest normally.7 The lips
and fingernails may demonstrate the classic signs of anoxia as they begin to
show a blue tint.7
Medical examination of
patients with croup reveals a narrowing of the subglottic area with edema,
resulting in a radiologically identifiable abnormality known as the "steeple
sign."1 The child's airway is at its most narrow in the
subglottic area. For this reason, any inflammation or narrowing in this
location is highly likely to cause airway compromise.6
Croup seldom causes serious
sequelae.7 Only about 1.3% to 2.6% of patients require
hospitalization.4,9 The duration of croup is typically three to
five days.7 A mild cough may persist for several days after the
most serious symptoms have regressed. There is an association between a
history of croup and asthma, but it is unclear which is causal for the other.
In one study, a recent diagnosis of croup (within one year of the survey)
almost doubled the risk for asthma.11
Treatment of Croup
Many patients with
croup have mild cases that can be treated at home, but there are exceptions.7
Patients should be urged to see a physician if the child's lips and
fingernails are blue, if there is evident trouble breathing, if drooling or
trouble swallowing is present, if the child is restless or confused, or if
vapor therapy does not result in improvement.7 Patients with
cyanosis, extreme pallor, agitation, or decreased awareness of their
surroundings, or those who are becoming fatigued from the effort of breathing,
should be given supplemental oxygen immediately.10
Croup of bacterial origin
requires appropriate antibiotic therapy. If the patient has stridor at rest,
physicians often admit the patient to the hospital until the stridor has
halted.12 Steroid therapy is usually effective in reversing the
stridor, perhaps as soon as six hours after therapy is begun.12,13
Inhaled steroids are often used.9 Oral prednisolone in a dose of 1
mg/kg is often effective.12 In a randomized trial, investigators
discovered that a single dose of dexamethasone (0.6 mg/kg) was effective in
speeding resolution of mild croup in children.14 A Cochrane
analysis revealed that steroids reduce symptoms and readmissions to emergency
departments, shorten hospital stays, and reduce the need for treatment with
epinephrine.3
Most children with croup have
a mild case, and they appear to be normal in observable behaviors such as
hunger and thirst, they engage in play activities, and they display their
usual disposition.10 Standard treatment for most mild cases of
croup is inhaled vapor therapy to ensure that airway secretions retain
adequate hydration.5 One physician suggests that parents/caregivers
take the child into a steamy bathroom, as the moisture will improve the
condition.8 While conceding that the suggestion may not be fully
reference based, the physician asserts that steam "carries the weight of
decades of practice." Another suggestion is to place a clean, wet washcloth
over the nose and mouth, so each breath becomes humidified.7
Patients are often advised by
physicians to humidify the child's bedroom with a vaporizer or humidifier.
Pharmacies usually stock an array of humidification devices, ensuring that
patients can obtain a product that meets their needs.
Steam vaporizers are available
in several configurations. Electrode vaporizers require filling a reservoir to
the indicated point, followed by placement of a boiling chamber into the
reservoir. Steel or carbon electrodes within the boiling chamber are immersed
in the water when the boiling chamber is placed into the reservoir. When the
outlet is connected to electricity, elements normally found in water (e.g.,
calcium, magnesium, iron) serve to conduct the electricity between the
electrodes, heating the water. After a short period, the heated water exits
the vaporizer outlet as sterile steam. If the water is excessively soft, the
patient should add electrolyte to the water. Some companies advise salt, while
others advise baking soda. The purchaser should be encouraged to read the
product brochure in order to determine the recommended electrolyte and the
suggested amount to add. On the other hand, if the water already contains
excessive electrolyte, some vaporizers eject boiling water from the steam
outlet. In these cases, the consumer should be advised to dilute household
water with distilled water until boiling water is no longer ejected.
Other vaporizers function by
heating the water with a heating element. The amount of electrolyte is not an
issue in steam generation, since the heating element is not dependent on it.
Both types of vaporizers
produce heated mist that can alleviate croup. Because steam has the potential
to burn, all vaporizers should be placed at least 4 feet from patients. They
should also be placed away from household traffic flow, such as in a corner
away from doors. The patient may choose to use medication with a vaporizer.
Several brands are available, containing volatile oils that have been proven
safe and effective for cough through the FDA review process.
Patients may choose cool-mist
humidifiers to humidify their child's room. The traditional type has a
reservoir into which a rapidly rotating spindle is immersed. As the spindle
rotates, water in the reservoir is drawn upward onto a spinning disk, which
breaks it down into small droplets. The fan action of the disk disperses the
water into the room. Patients may also purchase ultrasonic humidifiers--devices
that use ultrasonic technology to create an ultrafine mist. Distilled water is
optimal for both types of humidifiers, as electrolyte in the water droplets
can produce an annoying white dust of calcium and other electrolytes on
surfaces. The white dust can interfere with electronic equipment (e.g.,
computers, VCRs) if the humidifier is allowed to run too close to them.
Croup is worsened by agitation
or crying.4 Thus, parents should be urged to make the child as
comfortable as possible under the circumstances.
Prevention of Croup
As croup is a
transmissible respiratory disease, prevention steps are those usually employed
in the prevention of similar conditions, like the common cold and influenza.7
People should wash their hands often, keeping fingers away from the nose and
mouth. Any potentially infected facial tissues should be handled as infectious
materials and should be discarded immediately and not handled by others. Toys
or other objects that have been mouthed by a child with croup should be washed
to eliminate pathogens. Visitors or relatives with cough should avoid holding
or playing with children in the home.
References
1. Nakayama JM,
Tokeshai J. A case report of adult croup: a new old problem.
2. Knutson D, Aring A. Viral croup. Am Fam Physician. 2004;69:535-540.
3. Schooff M. Glucocorticoids for treatment of croup. Am Fam Physician. 2005;71:66-67.
4. Leung AK, Kellner JD, Johnson DW. Viral croup: a current perspective. J Pediatr Health Care. 2004;18:297-301.
5. Khater F, Moorman JP. Complications of influenza. South Med J. 2003;96:740-743.
6.
7. Information from your family doctor. What should I know about croup? Am Fam Physician. 2004;69:541-542.
8. Klass P. Croup--the bark is worse than the bite. N Engl J Med. 2004;351:1283-1284.
9. Baines PB, Sarginson RE. Upper airway obstruction. Hosp Med. 2004;65:108-111.
10. Fitzgerald DA, Kilham HA. Croup: assessment and evidence-based management. Med J Aust. 2003;179:372-377.
11. Cagney M, MacIntyre CR, MacIntyre PB, Peat J. Childhood asthma diagnosis and use of asthma medication. Aust Fam Physician. 2005;34:193-196.
12. Parker R, Powell CV, Kelly AM. How long does stridor at rest persist in croup after the administration of oral prednisolone? Emerg Med Australas. 2004;16:135-138.
13. Hiramanek N. Answering a question about the treatment of croup. Aust Fam Physician. 2005;34:171.
14. Custer JR. A randomized trial of a single dose of oral dexamethasone for mild croup. J Pediatr. 2005;146:434-435.

To comment on this article, contact editor@uspharmacist.com






