US Pharm.
32(11)12-15.
The potential number of
interactions between nonprescription products and psychotropic medications is
difficult to estimate due to the number of OTC products and the immense
probability that many will interact with psychotropics. Known or suspected
interactions fall into two categories. One is the group of OTC/psychotropic
interactions that were considered to be of such gravity that the FDA required
a warning label on the products. However, there is a second group composed of
interactions that are not found on the labeling of any nonprescription product.
Monoamine Oxidase Inhibitor
Warnings
In the late 1970s,
a specific group of medications was indicated for depression or hypertension:
monoamine oxidase inhibitors (MAOIs). At that time, several were actively
marketed as single-entity or combination products, including pargyline
(Eutonyl) and pargyline/methyclothiazide (Eutron) for hypertension and
phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan)
for depression. Eventually, selegiline (Eldepryl, Emsam) was marketed, with
enhanced affinity for MAOI type B active sites. It was referred to as an MAOI
"B" medication, and the older products became known as MAOI "A" medications.
Eutonyl, Eutron, and Marplan are no longer marketed.
Regarding MAOI therapy, one
set of precautions is paramount. MAOIs block the body's ability to metabolize
tyramine, carrying a high potential for drug and food interactions. Patients
prescribed MAOIs are cautioned strongly against ingestion of tyramine-rich
foods and drinks, such as anchovies, certain alcoholic beverages (e.g.,
sherry, beer), pepperoni, salami, strong/aged cheeses, raisins, bananas, and
soy sauce. Failure to observe this precaution can cause cerebral hemorrhages
and severe headaches.
When the nonprescription
cough/cold expert panel originally appointed by the FDA issued its report in
1976, it indicated evidence of the same type of interaction between MAOIs and
oral nasal decongestants (e.g., pseudoephedrine, phenylephrine,
phenylpropanolamine).1 In the panel's words, "Patients taking other
drugs whose action can intensify the sympathomimetic drug action, e.g.,
monoamine oxidase inhibitors, should not take nasal decongestants orally
except under the advice and supervision of a physician. The Panel does not
feel these restrictions should apply to topically applied nasal decongestants
when administered in recommended doses because of their localized action,
i.e., minimal systemic absorption." Accordingly, the panel recommended the
following labeling for oral nasal decongestants: "Drug Interaction Precaution:
Do not take this product if you are presently taking a prescription
antihypertensive or antidepressant drug containing a monoamine oxidase
inhibitor except under the advice and supervision of a physician." In 1985,
the FDA issued its Tentative Final Monograph for nasal decongestants.2
In responding to requests that the warning be clarified for consumers, FDA
suggested similar labeling: "Do not take this product if you are presently
taking a prescription drug for high blood pressure or depression, without
first consulting your doctor." Identical labeling was also proposed for other
nonprescription products containing sympathomimetic amines, such as
bronchodilator products with ephedrine or epinephrine for asthma.
In 1992, the FDA became aware of an
additional issue regarding MAOIs. Dextromethorphan was found to be a possible
cause of a potentially deadly interaction in patients taking MAOIs.3
Among the numerous cases reported, a 26-year-old female had been taking 15 mg
of phenelzine four times daily for a month but took a 30-mg dose after she
missed an earlier one. She also ingested 2 oz. of a
dextromethorphan-containing cough syrup, which led to nausea, dizziness, and
collapse. She was severely hypotensive when taken to the hospital, with a
systolic that did not rise above 70 mmHg and a temperature of 107.6 to 107.96°
F. She died of a cardiac arrest four hours postadmission.
A 15-year-old female taking 15
mg of phenelzine three times daily for depression took eight capsules
containing 15 mg of dextromethorphan, 6.25 mg of phenindamine, and 5 mg of
phenylephrine, followed by another five capsules three hours later. She was
found to have fixed, dilated pupils, lack of a gag reflex, mild spasticity,
and hyperreflexia of the upper limbs. Resuscitation efforts were unsuccessful.
Her autopsy revealed acute cerebral edema, marked acute pulmonary edema, and
hemohydrothorax.
The FDA observed that
prescribing of MAOIs had increased in the years preceding 1992. Thus, FDA
proposed in the 1992 document to extend the MAOI warning to dextromethorphan,
with wording as follows, "Do not use this product if you are taking a
prescription drug containing a monoamine oxidase inhibitor (MAOI) (certain
drugs for depression or psychiatric or emotional conditions), without first
consulting your doctor. If you are uncertain whether your prescription drug
contains an MAOI, consult a health professional before taking this product."
In 1993, the FDA published the final monograph on this topic, including a
discussion of the comments it had received.4 In response to two
such comments, the agency decided to include selegiline as a possible source
of drug interactions, to require a reference to selegiline's use in
Parkinson's disease, and to indicate that a two-week washout period should be
observed. The final label required by the FDA reads: "Do not use this product
if you are now taking a prescription monoamine oxidase inhibitor (MAOI)
(certain drugs for depression, psychiatric or emotional conditions, or
Parkinson's disease), or for 2 weeks after stopping the MAOI drug. If you are
uncertain whether your prescription drug contains an MAOI, consult a health
professional before taking this product." The proposed labels for nasal
decongestants and bronchodilators for asthma were identical to that proposed
for dextromethorphan, as well as in the final monograph that eventually
appeared for bronchodilators.
The FDA Panel assigned to
review anorectal products recognized in its 1980 report that topical
vasoconstrictors in hemorrhoid products (e.g., phenylephrine) could be
absorbed in sufficient quantities to interact with MAOIs.5 The
FDA-required label for these products is not as complete as the labels above,
stating only, "Ask a doctor or pharmacist before use if you are presently
taking a prescription drug for high blood pressure or depression."6
Furthermore, the label ignores the use of selegiline for Parkinson's disease.
Additive Sedation
Brompheniramine,
chlorpheniramine, clemastine, cyclizine, dexbrompheniramine, dimenhydrinate,
doxylamine, meclizine, phenindamine, pheniramine, pyrilamine, and triprolidine
must carry warnings advising the patient about possible drowsiness if they are
taken concurrently with alcohol, sedatives, or tranquilizers.6
Diphenhydramine products also carry this warning but must state that they can
cause "marked drowsiness." These ingredients are found in products indicated
for allergic rhinitis, the common cold, motion sickness, insomnia, and
menstrual discomfort.
Nicotine and Prescription
Antidepressants
Nonprescription
nicotine cessation products carry a specific warning against concurrent use
with prescription antidepressants unless the patient first speaks to a
physician or pharmacist. This warning appears on nicotine gum, patches, and
lozenges and is required because cessation of smoking can increase the plasma
concentrations of some antidepressant medications.6
Omeprazole and Diazepam
Nonprescription
omeprazole carries a drug interaction warning against concomitant use with
diazepam.6 Omeprazole can inhibit the metabolism of diazepam,
elevating its blood concentrations.
Global Warnings Against Use
with Prescription Products
Several
nonprescription medications contain nonspecific warnings against use with any
prescription product without a pharmacist or physician's advice, which of
necessity would include all psychotropic medications. They include naproxen,
ibuprofen, and codeine-containing schedule V cough syrups.6 As an
example of the importance of these warnings, naproxen and ibuprofen both
increase serum lithium levels when given concurrently with it.7
A global precaution also
applies to medications that could alter the absorption of others, such as
psyllium. One manufacturer warns against taking any other prescription
medication two hours before or two hours after ingesting psyllium, as the
medication may be trapped in the psyllium matrix and unavailable for
absorption.6
Nonlabeled Psychotropic
Interactions
The medical
literature mentions numerous potential interactions between nonprescription
products and psychotropic medications. Despite their inclusion in the
literature, many are not included on the FDA-required label. Thus, the patient
contemplating purchase of products without physician advice encounters no
label warning and can rely only on the help of an informed pharmacist. For
instance, cimetidine can interact with benzodiazepines, a fact not required on
the cimetidine label.
Dietary supplements seldom, if
ever, carry drug interaction warnings. Nevertheless, they can be the source of
interactions with psychotropic medications. The following have been observed:
St. John's wort and other SSRI antidepressants (serotonin syndrome); St.
John's wort and lowered plasma concentration when used with amitriptyline,
alprazolam, or midazolam; black cohosh and sedatives/hypnotics; capsicum and
barbiturates or MAOIs; cat's claw and Halcion; chamomile and benzodiazepines
or sedatives; coenzyme Q10 and phenothiazines or tricyclics; ephedra and MAOIs
or tricyclics; eucalyptus and amphetamines or barbiturates; fish oil and
antipsychotics; gingko and MAOIs; ginseng and MAOIs or stimulants; and kava
and numerous psychotropics.7-10

References
1. Establishment of
a monograph for OTC cold, cough, allergy, bronchodilator and antiasthmatic
products. Fed Reg. 1976;41:38312-38424.
2. Cold, cough,
allergy, bronchodilator, and antiasthmatic drug products for over-the-counter
human use. Tentative final monograph for over-the-counter nasal decongestant
drug products. Fed Reg. 1985;50:2220-2241.
3. Cold, cough,
allergy, bronchodilator, and antiasthmatic drug products for over-the-counter
human use. Proposed amendment of final monograph for OTC antitussive drug
products. Fed Reg. 1992;57:27666-27670.
4. Cold, cough,
allergy, bronchodilator, and antiasthmatic drug products for over-the-counter
human use. Amendment of final monograph for OTC antitussive drug products.
Fed Reg. 1993;58:54232-54236.
5. Anorectal drug
products for over-the-counter human use; Establishment of a monograph. Fed
Reg. 1980;45:35576-35677.
6. Pray WS.
Nonprescription Product Therapeutics, 2nd ed. Baltimore, MD: Lippincott
Williams & Wilkins; 2005.
7. Honig PK, Gillespie
BK. Drug interactions between prescribed and over-the-counter medication.
Drug Saf. 1995;13:296-303.
8. Clark A. Finding
health in folklore, herbs, and supplements: The good, the bad & the ugly. Part
III--the ugly. Mo Med. 2003;100:91-93.
9. Pal D, Mitra AK.
MDR- and CYP3A4-mediated drug-herbal interactions. Life Sci.
2006;78:2131-2145.
10. Magee K, Loiacono
C. A review of common herbs and potential interactions. Int J Dent Hyg.
2004;2:111-121.
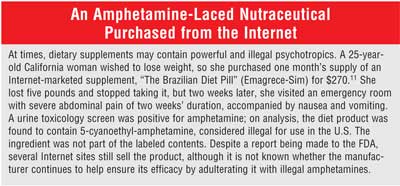
11. Nguyen MH, Ormiston
T, Kurani S, et al. Amphetamine lacing of an Internet-marketed neutraceutical
(sic). Mayo Clin Proc. 2006;81:1627-1629.
To comment on this article, contact
editor@uspharmacist.com.






