US Pharm.
2006;11:HS-44-HS-52.
A woman
in labor is commonly referred to as a parturient in the medical
literature. The parturient may be offered various medications to alleviate
labor pains. Medications given for analgesia in labor will decrease the pain
sensation, while medications used for anesthesia should provide complete pain
relief.1 Women of today, especially those living in the United
States, certainly have more options than their mothers and grandmothers did.
Stages of Labor
There are three
stages of labor. The first begins with the onset of labor, as a woman
experiences general abdominal cramping and uterine contractions. Once the
cervix has completely dilated, the second stage of labor begins. The woman
begins pushing during contractions, with the stage ending when the baby is
delivered. Pain in the second stage of labor may be more intense and
continuous. During the third stage, the placenta is delivered.2
Labor pain is affected by
nerves near the lower thoracic spinal segments (10-12) and the first lumbar
spinal segment. Medication administered into either the epidural or
subarachnoid spaces can block the pain.3
A woman's perception of labor
pain is affected by many factors, including cultural, psychosocial,
environmental, and physiologic influences. Nulliparous women may have more
pain in early labor, while women who have gone through childbirth previously
note more pain in the late first stage and second stage.
Early Use of Labor Analgesia
Early Chinese
documents describe the first use of an opioid, opium, in treating labor pain.4
Two British obstetricians pioneered the use of ether as an inhalational
anesthetic for labor pain in the 1840s. Chloroform eventually became the
anesthetic of choice in place of ether.5 In 1902, morphine and
scopol amine use for labor pain was reported. There was little benefit in
pain relief, although the "twilight sleep" caused maternal confusion and
forgetfulness of the event. However, these drugs were also associated with
neonatal respiratory depression.6 Meperidine came into use during
the early 1940s, eventually becoming the most regularly used opioid for labor
pain worldwide.7
The first reported case of
regional anesthesia used in labor occurred in 1900, when a physician from
Switzerland administered spinal cocaine to six of his patients. Two years
later, spinal anesthesia was used for the first time for a cesarean delivery
in the U.S.8 In the late 1960s, epidural analgesia became more
accepted, especially among academic health centers and private hospitals.
Nonpharmacologic
Interventions
There are multiple
nonpharmacologic techniques used to reduce labor pain. These interventions
include acupuncture, massage, intracutaneous sterile water blocks, water
immersion or hydrotherapy, music or audioanalgesia, cold or heat therapy,
hypnosis, breath ing/focusing, and transcutaneous electrical nerve
stimulation.9 However, a primary disadvantage of alternative or
nonpharmacologic techniques is the lack of rigorous research to support their
use. Advantages to nonpharmacologic interventions include their low cost and
wide availability and the fact that they pose low or no risk to the mother and
neonate and allow active participation of the mother throughout the labor
process.
Routes of Analgesia
Administration
There are several
routes of analgesia administration used to reduce labor pain. These routes
include intravenous (IV), intramuscular (IM), subcutaneous, paracervical
blocks, epidural, spinal, and combined spinal epidural.
Parenteral Routes:
Opioid derivatives are the agents used for IV and IM analgesia. These agents
may moderately reduce labor pains, but they cannot eradicate the pain. IV
administration provides a faster onset of analgesia with a shorter duration of
action, while IM administration should be considered when pain relief for a
longer duration is needed (see Table 1).1 Common side
effects of opioids include constipation, dry mouth, urinary retention,
sedation, nausea, vomiting, dysphoria, hypoventilation, pruritus, and neonatal
depression.1 Several studies have evaluated the benefits of IV
analgesia. Soontrapa et al. reported that fewer than 25% of those receiving an
IV opioid analgesic had adequate pain relief.10
Parenteral use of opioids may
be warranted in those patients who have contraindications to epidural
analgesia; previous spinal surgery or deformity, which may make it impossible
to place an epidural; or the unavailability of anesthesia or personnel
services.
Morphine was the first pure
opioid given for relief of labor pain. Doses ranged from 1 to 4 mg with a peak
effect at 20 minutes after IV administration. The peak effect for IM dosing
was delayed to one to two hours. Side effects with morphine include maternal
and neonatal respiratory depression and maternal nausea, vomiting, and
sedation. Morphine is rarely used during labor in the U.S. because of its long
half-life, high incidence of sedation, and neonatal side effects.11
In the 1940s, meperidine came
into use for labor analgesia and is now the most frequently used opioid for
labor pain. IV doses are typically 25 to 50 mg and IM doses are 50 to 100 mg.
It has a faster onset of action--five to 10 minutes for IV dosing and 45
minutes for IM dosing--than morphine does. As with morphine, meperidine can
cause neonatal respiratory depression. The significance of this effect depends
on the dose given, as well as the time between dose administration and
delivery. A neonate is less likely to suffer respiratory depression if
delivery occurs one hour after dosing or more than four hours after dosing.
The strongest effects on the neonate tend to occur if delivery takes place two
to three hours after the meperidine dose is given. Another disadvantage of
meperidine is its metabolism to normeperidine in the neonate, as this
metabolite has a much longer half-life (63 hours).11,12
Fentanyl, a synthetic opioid,
has several advantages over morphine and meperidine. It has a rapid onset of
action of only one to two minutes when it is given intravenously and a short
duration of action of 60 minutes. IM and IV doses range from 50 to 100 mcg.1,12
Fentanyl does not readily cross the placenta, as morphine and meperidine do;
however, neonatal respiratory depression may still occur. Fentanyl has been
noted to cause less maternal sedation, nausea, vomiting, and pruritus as
compared to morphine and meperidine.
Butorphanol, an opioid
agonist-antagonist, is given in doses of 1 to 2 mg IV or IM. It has an onset
of action of two to three minutes after IV dosing and 10 to 30 minutes after
IM dosing. It has a three- to four-hour duration of action with either IV or
IM administration.1,12 Another opioid agonist-antagonist is
nalbuphine, which can be given as either an IV or IM10-mg dose. It has a
slightly faster peak effect of two to three minutes when given intravenously
and 15 minutes after IM dosing.1,12 Both butorphanol and nalbuphine
may cause maternal respiratory depression.1 Patients who may take
narcotics for other medical conditions or who are drug abusers may experience
withdrawal symptoms due to the antagonistic effects of butorphanol and
nalbuphine.11

Paracervical Blocks: Paracervical block was a method commonly used in the 1940s and 1950s; however, its use has decreased with the increasing availability of epidural analgesia. A paracervical block involves the injection of local anesthetics, such as lidocaine or bupivacaine, into either side of the cervix. A major disadvantage seen with paracervical blocks is fetal bradycardia. When this procedure was first implemented, fetal bradycardia was reported to occur 70% of the time.13 However, this incidence has dropped to a rate of 15% with present methods.14
Regional Analgesia: Regional analgesia includes epidural, spinal, and combined spinal and epidural procedures that result in partial to complete loss of pain sensation below the T8 to T10 levels of the spine (see Table 2 for contraindications to regional anesthesia).12 In the U.S., there are four million births each year, and nearly 60% of women giving birth receive an epidural.15 Epidural procedures require administration of analgesics or anesthetics via catheter into the area of fibrous connective tissue (dura mater) covering the spinal cord. Spinal analgesia requires piercing the dura into the cerebrospinal fluid–filled cavity, where the spinal cord is located.11 Spinal analgesia is a single dose of a long-acting local anesthetic with or without an opioid agent. For spinal analgesia, small doses of medications are required (e.g., fentanyl 25 mcg with 1 mL bupivacaine 0.25%), whereas, larger doses are needed for epidural use (e.g., fentanyl 50 to 100 mcg with 10 to 15 mL bupivacaine 0.125% to 0.25%).3

Combined spinal and epidural
analgesia is a more recent technique that offers the benefit of spinal
analgesia's quick onset of action, along with the ability to provide an
epidural for an extended period. Combined spinal and epidural administration
is accomplished via a "needle-through-needle" technique. Medication is
injected via the spinal needle into the subarachnoid space. The spinal needle
is removed, leaving the epidural needle in position, and the epidural catheter
is threaded through.1 Within three to five minutes, analgesia
begins with a duration of 60 to 90 minutes. As the spinal analgesia fades, the
anesthesiologist can use the epidural catheter during the remainder of the
labor process.
Continuous infusion of an
anesthetic with an opioid is commonly used in labor. Continuous infusions
offer a more steady level of pain control, compared to bolus administrations.
These infusions typically contain bupivacaine or ropivacaine 0.04% to 0.125%
and fentanyl or sufentanil.3
Factors that affect rates of
epidural use include availability of anesthesia services, conditions or
criteria for use (e.g., stage of labor or patient demand), and the size of the
hospital.16 Currently, there is debate in the medical literature on
whether epidurals should be given early in labor rather than later and what
effects this may have on the labor process and delivery. In hospitals with
delivery rates of at least 1,500 births per year, the percentage of patients
getting epidurals jumped from 22% to 51% from 1981 to 1992.17
Medications given epidurally
include opioid analgesics, anesthetics, or more commonly, both. The
combination has an additive effect.18 Analgesics commonly used for
epidurals include fentanyl and sufentanil, which are better tolerated than
morphine and meperidine. The drawbacks for epidural morphine are its long
onset time and modest effectiveness.
Local anesthetics used in
regional anesthesia include low-dose cocaine derivatives: bupivacaine,
lidocaine, and ropivacaine.11 Common side effects include pruritus,
inability to urinate, and hypotension.
Bupivacaine is a commonly used
local anesthetic, and its advantages include prolonged duration of action, low
placental transfer, and efficacy in both early and late stages of labor.19
Bupivacaine was the first anesthetic of choice for several decades; however,
it fell out of favor in the mid-1980s after several maternal deaths due to
cardiotoxicity of bupivacaine 0.75% solution.20
Lidocaine is used less often
than bupivacaine because it offers less pain relief and has a shorter duration
of action.11 On the other hand, it has a decreased risk of
cardiotoxicity compared to bupivacaine.
Ropivacaine is similar to
bupivacaine in onset, duration, and sensory block; however, ropivacaine is the
S-enantiomer, and bupivacaine is a racemic mixture of both the R and S forms.21
Ropivacaine, like lidocaine, has less risk of cardiotoxicity than does
bupivacaine. Ropivacaine use also reduces the need for instrumental vaginal
deliveries. A meta-analysis by Writer et al. noted a 13% reduction in
instrumental vaginal deliveries with ropivacaine use compared to bupivacaine.22
Efficacy of ultra-low-dose
epidurals and combined spinal epidurals, which are referred to as walking
epidurals, was evaluated in several studies. Low concentrations of
bupivacaine or ropivacaine in combination with fentanyl allowed for sufficient
analgesia along with the majority of patients retaining the ability to
ambulate. A study by Breen et al. noted that low-dose bupivacaine at 0.04%
with fentanyl and epinephrine produced sufficient analgesia with little motor
impairment.23 Campbell et al. reported that 100% of patients
receiving epidural ropivacaine 0.08% with fentanyl 2 mcg/mL were able to
continue ambulating, compared to 75% of the patients receiving bupivacaine
0.08% with fentanyl 2 mcg/mL.24
There are several precautions
to consider for the laboring woman who wishes to ambulate. The patient's blood
pressure as well as fetal heart rate should be monitored for 30 to 60 minutes
after initiation of the epidural and then at least every 30 minutes
thereafter. The patient should demonstrate her ability to walk by either
stepping up and down on a stool or performing knee bends. Finally, the patient
should never ambulate alone.2
Maternal and Labor Effects
of Regional Analgesia
Studies have noted that epidural use is associated with negative effects (see Table 3): increased length of the first and second stages of labor, increased use of forceps or vacuum in deliveries, and maternal fever.
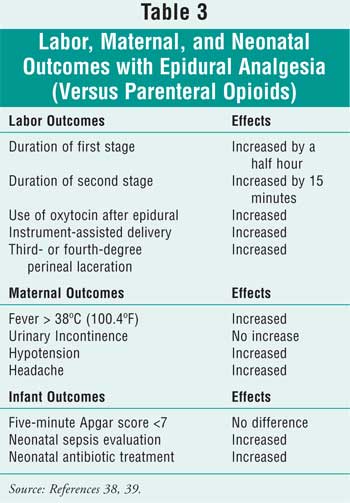
There have also been concerns that
epidural use increases the need for cesarean delivery. Two separate
meta-analyses noted no change in cesarean rates between epidural and
parenteral opioid groups; however, first and second stages of labor were
prolonged in patients in the epidural groups compared to those in the
parenteral opioid groups.25,26 Several studies by Chestnut et al.
have shown that higher concentrations of bupivacaine (0.125% vs. 0.0625% +
0.0002% fentanyl) given epidurally can cause significant motor blockade and
increase the risk of forceps delivery.27-29
Epidural analgesia in labor is
frequently linked to maternal fever with a body temperature higher than 100.4ºF.
One randomized trial observed that 15% of women who received an epidural had a
fever, as compared to only 4% of those who did not receive an epidural. This
percentage increased for those nulliparous women in the study (24% vs. 5%).30
Neonates born to mothers who have received epidurals are more often assessed
and treated with antibiotics due to concerns of possible infection.31
Another concern with epidurals
is puncture of the subarachnoid space during positioning of the epidural
needle. This early complication causes a minuscule quantity of spinal fluid to
seep out into the epidural space, leading to a postdural headache.11
Punctures occur in about 3% of women and account for 70% of severe headaches
in postpartum women.32
General Anesthesia
General
endotracheal anesthesia for emergency cesarean delivery is indicated when
there is severe fetal distress with insufficient time to establish regional
anesthesia, as well as cases of coagulopathy, severe maternal hemorrhage, or
failure of regional anesthesia.1
General anesthesia involves
injection of a rapid-acting induction agent such as thiopental, ketamine, or
etomidate and a short-acting muscle relaxant such as succinylcholine or
rocuronium to cause deep sedation and analgesia, as well as muscle paralysis
and apnea. A tracheal tube is placed, and anesthesia is maintained with
oxygen, an inhalational agent, and nitrous oxide.33
Failure of tracheal intubation
in obstetric patients is nearly 10 times that in nonobstetric patients.34
Capillary swelling of the mucosa in the trachea due to pregnancy reduces the
internal space of the trachea. Anesthesia-related maternal death is the sixth
leading cause of pregnancy-associated deaths in the U.S.35 The
fatality rate for general anesthesia in cesarean delivery is projected at 32
per one million live births versus 1.9 per one million live births for
regional anesthesia.36
Summary
The American
College of Obstetricians and Gynecologists offered this statement in a recent
bulletin: "Labor results in severe pain for many women. There is no other
circumstance in which it is considered acceptable for a person to experience
untreated severe pain, amenable to safe intervention, while under a
physician's care. In the absence of a medical contraindication, maternal
request is a sufficient medical indication for pain relief during labor. Pain
management should be provided whenever it is medically indicated."12
For women suffering from labor
pain, there are many choices available for pain relief. The route of pain
relief will depend on specific circumstances for each patient and the level of
pain experienced.
References
1. Poole JH. Analgesia and anesthesia during labor and birth: implications for mother and fetus. J Obstet Gynecol Neonatal Nurs. 2003;32:780-793.
2. Gaiser RR. Labor epidurals and outcome. Best Pract Res Clin Anesthesiology. 2005;19:1-16.
3. Belin Y. Advances in labor analgesia. Mount Sinai J Medicine. 2002;Jan/March:38-43.
4. Harmer M, Rosen M. Parenteral opioids. In: Van Zundent A, Ostenheimer GW, eds. Pain Relief and Anaesthesia in Obstetrics. Churchill Livingstone; 1996:365-372.
5. Caton D. Obstetric anesthesia: the first ten years. Anesthesiology. 1970;33:102-109.
6. Von Steinbuchel. Vorlaufige mittheilung uber die anwendung von skopolamin-morphium-injectionem in der Gerburtshilfe. Zentrabl F Gynok. 1902;26:1304.
7. Bricker L, Lavender T. Parenteral opioids for labor pain relief: a systematic review. Am J Obstet Gynecol. 2002;186:S94-S109.
8. Gogarten W, Van Aken H. A century of regional analgesia in obstetrics. Anesth Analg. 2000;91:773-775.
9. Simkin P, Bolding A. Update on nonpharmacologic approaches to relieve labor pain and prevent suffering. J Midwifery Women's Health. 2004;49:489-504.
10. Soontrapa S, Somboonpron W, Komwilaisak R, et al. Effectiveness of intravenous meperidine for pain relief in the first stage of labour. J Med Assoc Thai. 2002;85:1169-1175.
11. Althaus J, Wax J. Analgesia and anesthesia in labor. Obstet Gynecol Clin N Am. 2005;32:231-244.
12. ACOG Practice Bulletin No. 36. Clinical management guidelines for obstetrician-gynecologists. Obstetric Analgesia Anesthesia. 2002;100:177-191.
13. Manninen T, Aantaa R, Salonen M, et al. A comparison of the hemodynamic effects of paracervical block and epidural anesthesia for labor analgesia. Acta Anaesthesiol Scand. 2000;44:441-445.
14. Rosen MA. Paracervical block for labor analagesia: a brief historic review. Am J Obstet Gynecol. 2002;186(5 Suppl):S127-S130.
15. Eltzschig HK, Lieberman ES, Camann WR. Regional anesthesia and analgesia for labor and delivery. N Engl J Med. 2003;348:319-332.
16. Yancey MK, Pierce B, Schweitzer D, et al. Observations on labor epidural analgesia and operative delivery rates. Am J Obstet Gynecol. 1999;180(2 Pt 1):353-359.
17. Hawkins JL, Gibbs CP, Orleans M, et al. Obstetric anesthesia work force survey, 1981 versus 1992. Anesthesiology. 1997;87:135-143.
18. Lim Y, Sia AT, Ocampo CE. Comparison of intrathecal levobupivacaine with and without fentanyl in combined spinal epidural for labor analgesia. Med Sci Monit. 2004;10:187-191.
19. Belfrage P, Berlin A, Raabe N, et al. Lumbar epidural analgesia with bupivacaine in labor: drug concentration in maternal and neonatal blood at birth and during the first day of life. Am J Obstet Gynecol. 1975;123:839-844.
20. Kuczkowski K. Levobupivacaine and ropivacaine: the new choices for labor analgesia. Int J Clin Pract. 2004;58:604-605.
21. Drysdale SM, Muir H. New techniques and drugs for epidural labor analgesia. Sem Perinatology. 2002;26:99-108.
22. Writer WD, Stienstra R, Eddleston JM, et al. Neonatal outcome and mode of delivery after epidural analgesia for labour with ropivacaine and bupivacaine: a prospective meta-analysis. Br J Anaesth. 1998;81:713-717.
23. Breen TW, Shapiro T, Glass B, et al. Epidural anesthesia for labor in an ambulatory patient. Anesth Analg. 1993;77:919-924.
24. Campbell DC, Zwack RM, Crone LA, et al. Ambulatory labor epidural analgesia: bupivacaine versus ropivacaine. Anesth Analg. 2000;90:1384-1389.
25. Halpern SH, Leighton BL, Ohlsson A, et al. Effect of epidural vs. parenteral opioid analgesia on the progress of labor. A meta-analysis. JAMA. 1998;280:2105-2110.
26. Sharma SK, McIntire DD, Wiley J, Leveno KJ. Labor analgesia and cesarean delivery: an individual patient meta-analysis of nulliparous women. Anesthesiology. 2004;100:142-148.
27. Chestnut DH, Vandewalker GE,
Owen CL, et al. The influence of continuous epidural bupivacaine analgesia on
the second stage of
labor and method of
delivery in nulliparous women. Anesthesiology. 1987;66:774-780.
28. Chestnut DH, Laszewski LJ, Pollack KL, et al. Continuous epidural infusion of 0.0625% bupivacaine – 0.0002% fentanyl during the second stage of labor. Anesthesiology. 1990;72:613-618.
29. Chestnut DH, Owen CL, Bates JN, et al. Continuous infusion epidural analgesia during labor: a randomized double-blind comparison of 0.0625% bupivacaine/0.0002% fentanyl versus 0.125% bupivacaine. Anesthesiology. 1988;68:754-759.
30. Philip J, Alexander JM, Sharma SK, et al. Epidural analgesia during labor and maternal fever. Anesthesiology. 1999;90:1271-1275.
31. Lieberman E, Lang JM, Frigoletto F Jr, et al. Epidural analgesia, intrapartum fever, and neonatal sepsis evaluation. Pediatrics. 1997;99:415-419.
32. Norris MC, Leighton BL, DeSimone CA. Needle bevel direction and headache after inadvertent dural puncture. Anesthesiology. 1989;70:729-731.
33. Mattingly JE, D'Alessio J, Ramanathan J. Effects of obstetric analgesics and anesthetics on the neonate. Pediatr Drugs. 2003;5:615-627.
34. Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42:487-490.
35. Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related mortality in the United States, 1987-1990. Obstet Gynecol. 1996;88:161-167.
36. Hawkins JL, Koonin LM, Palmer SK, Gibbs CP. Anesthesia-related deaths during obstetric delivery in the United States, 1979-1990. Anesthesiology. 1997;86:277-284.
37. Campbell DC. Parenteral opioids for labor analgesia. Clin Obstet Gynecol. 2003;46:616-622.
38. Lieberman E, O'Donoghue C. Unintended effects of epidural analgesia during labor: a systematic review. Am J Obstet Gynecol. 2002;186(Suppl 5):S31-S68.
39. Leighton BL, Halpern SH. The
effects of epidural analgesia on labor, maternal, and neonatal outcomes: a
systematic review. Am J Obstet Gynecol. 2002;186(Suppl 5):S69-S77.
To
comment on this article, contact editor@uspharmacist.com.






