US Pharm.
2007;32(7)(OTC suppl):13-17.
Acne vulgaris is a common skin disorder,
affecting 40 to 50 million people in the United States.1
Approximately 85% of the adolescent population will develop acne to some
degree, and 40% to 54% of individuals older than 25 are affected as well. The
incidence is generally universal among ethnicities and between genders, except
in the case of adult acne; approximately 3% of males are affected versus 12%
of females.2 Although acne is a self-limiting disorder that may
appear to be mostly cosmetic in nature, it may place an emotional and
psychological burden on the affected individual that is more than skin deep.
The physical change on the surface of the skin and, at times, the accompanying
scarring may lead to a reduction in quality of life comparable to that of
people with epilepsy, asthma, diabetes, or arthritis.3 The
psychologic impact, which can include social withdrawal, lack of confidence,
anxiety, and depression, has been associated with higher rates of unemployment.
1,3,4
In the U.S., the direct cost
of acne is estimated to be $1 billion per year; $1 million is spent on OTC
products.4 Considering the extensive marketing of these products
and the implications of increased self-confidence and clearer skin, the number
of available products is not surprising. Although 20% of all visits to
dermatologists are for the evaluation of acne, there are many patients who
purchase OTC products to clear and treat their acne.2 Therefore,
pharmacists have an important role in evaluating the patient; choosing the
best OTC therapeutic regimen, if appropriate; and counseling the patient about
necessary nonpharmacologic measures.
Pathogenesis of Acne
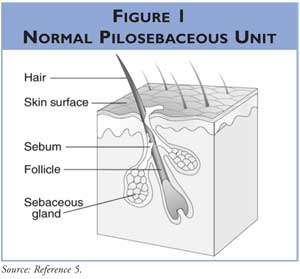
Acne is a disease
of the pilosebaceous units, which are found everywhere in the dermis (Figure 1) except the palms and soles.5 The face, upper back,
and chest have the highest density of these units. Each unit consists of a
hair follicle and sebaceous gland that produces sebum, an oily substance
containing free and esterified fatty acids and lipid components. There are
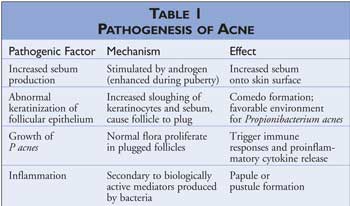
four primary factors involved in the pathogenesis of acne: increased sebum
production, abnormal keratinization of follicles, Propionibacterium acnes
proliferation, and inflammation (Table 1). The interplay of these four
factors causes the formation of acne lesions. The amount of sebum secreted may
correspond to the severity of acne. Sebum production is stimulated by androgen
circulation, and during puberty, there is increased androgenic activity. The
increase in sebum, combined with increased sloughing of keratinocytes (cells
lining the follicle) and hair, produces a plug in the narrow follicle. P
acnes normally resides on the dermis; however, the mixture of sebum and
cells provides the bacterium with an environment that facilitates
proliferation in the plugged follicles. This in turn may cause inflammation, a
consequence of the bacteria producing biologically active mediators and
promoting proinflammatory cytokine release.1,2,5-7
External factors that exacerbate acne include high humidity; local
irritation/friction (e.g., occlusive clothing, headbands, hand resting on
face); dirt, vaporized cooking oils, chemicals; oil-based cosmetics/hair
products; moisturizers/tanning oils with comedogenic oils (i.e., lanolin,
mineral oil, cocoa butter); medications (i.e., phenytoin, isoniazid,
phenobarbital, lithium, steroids, some oral contraceptives); and diet
(high-glycemic carbohydrates possibly lead to hormonal change).2,6
Internal factors that exacerbate acne include prolonged sweating, emotions
(i.e., stress), hormones (associated with menses), and heredity.2
Clinical Presentation
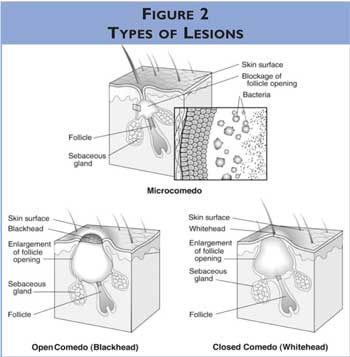
Clinically, acne presents as lesions that may be noninflammatory comedones,
either open or closed, or inflammatory pustules, erythematous papules, cysts,
nodules, or abscesses (Figure 2). The initial lesion is the closed
comedo, an enlarged and plugged hair follicle remaining beneath the skin, more
commonly known as a whitehead. An open comedo, known as a blackhead
, occurs when the contents of the follicle extrude. Rupturing of the
follicular wall may cause a more severe inflammatory reaction, discharging the
contents into the surrounding tissue. This would present as papules
(i.e., small, pink bumps on the skin) or pustules (i.e., white or
yellow pus filled papules that may be red at the base). More painful solid
lesions called nodules or deep pus-filled lesions called cysts
may occur and are more likely to leave scarring.
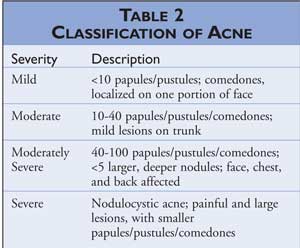
The diagnosis of acne is not difficult and is often made by the patient. Acne
is characterized by a variety of lesions, particularly on the face but also on
the neck, chest, shoulders, and back. Various systems are utilized to classify
the severity of acne, which take into account the number, type, and
distribution of comedones, papules/pustules, and nodules. The severity of acne
can range from mild to severe. Detailed description of the various grades of
acne is described in Table 2. Knowing the degree of severity allows the
pharmacist to evaluate the necessity of immediate referral to a physician and
choose the appropriate OTC therapy.2,4,7
Treatment
The treatment of acne involves a combination of both nonpharmacologic and
pharmacologic therapies.
Nonpharmacologic Therapy
Nonpharmacologic
methods for preventing and treating acne include avoiding/minimizing
exacerbating factors--such as restrictive clothing, resting hands on the face
and/or skin, using oil-based cosmetics, infrequent washing of oily hair,
exposure to environmental factors (i.e., dirt, chemicals)--and
picking/squeezing acne lesions.2 Patients should gently wash the
face twice daily to remove excess sebum from the skin. Cleaners with pumice,
polyethylene, or aluminum oxide may irritate the skin, producing inflammatory
lesions, and should be avoided. In addition, antimicrobial soaps should be
avoided, since they have no proven clinical value.
Pharmacologic Therapy
Benzoyl peroxide, salicylic acid, sulfur, sulfur with resorcinol, and several
herbal remedies are available OTC to treat mild-to-moderate acne. There are
numerous products bearing different names, dosage forms, and advertising
claims; however, most contain one or more of the aforementioned active
ingredients. Mechanistically, these various agents target the four pathogenic
factors. A product should be chosen based on maximum efficacy with minimal
adverse effects, as well as on targeting of the pathogenic factor.8
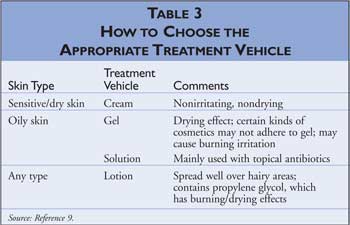
Because patients have differing skin types, the dosage form achieving the
greatest effect will vary among patients. Table 3 provides information
on selecting the appropriate dosage form for different skin types.
Benzoyl Peroxide:
Introduced in the 1960s, benzoyl peroxide is the most widely used topical
agent for acne. It is available in various dosage forms in concentrations of
2.5% to 20%. The maximum concentration available as an OTC product is 10%.
Benzoyl peroxide† has anti-inflammatory properties and is a bactericidal agent
that penetrates the dermis and enters the pilosebaceous follicle, generating
free radicals that oxidize proteins in the bacterial cell membrane and thereby
reduce P acnes. Studies have shown that the various strengths of
benzoyl peroxide have similar effectiveness; however, at equivalent strengths,
the gel form is superior to the lotion form, because the drying effect of the
alcohol in the gel enhances its effectiveness. Although P acnes has
demonstrated resistance to antibiotics, its resistance to benzoyl peroxide has
not been reported. Additionally, benzoyl peroxide has comedolytic effects due
to irritation of the skin, which causes an increased rate of sloughing of
epithelial cells. The comedolytic effect does not occur with washes and
cleansers.2,9-12
Adverse reactions include
excessive dryness, peeling, skin sloughing, erythema, and edema. These effects
may be reduced by using a lower strength of benzoyl peroxide. A transient
stinging or burning may occur. Additionally, bleaching of hair, clothing, and
bed linens may occur with the use of benzoyl peroxide.2
The FDA is determining the
safety of benzoyl peroxide. Warning statements have reported that benzoyl
peroxide is a tumor promoter and progressor, and safety studies are being
conducted to determine if it enhances ultraviolet radiationñinduced skin
cancer. Studies conducted in the late 1990s concluded that benzoyl peroxide
"is not carcinogenic in the skin or in ëselect internal organs' of mice and
rats [and] does not enhance photocarcinogenesis in mice."2
The active ingredient in two
parts of the three-step regimen of a popular product, Proactiv, is benzoyl
peroxide 2.5%. One study compared the efficacy of Proactiv with benzoyl
peroxide plus allylamine to possibly amplify effectiveness. Results indicated
that the benzoyl peroxide/allylamine combination was more effective than
Proactiv. Although this was a small-scale, open-label study, findings suggest
that benzoyl peroxide activity may be augmented with a tertiary amine such as
allylamine.13
Pharmacists should advise
patients that benzoyl peroxide is associated with increased sun sensitivity;
therefore, sunscreen should be thoroughly applied and reapplied as needed.
Additionally, benzoyl peroxide should be applied to dry skin once or twice
daily. Before titrating the dosage or deeming the product ineffective,
patients should keep in mind that maximum effects are seen in four to six
weeks.
Salicylic Acid:
Salicylic acid is a mild
comedoyltic agent that acts as a surface keratolytic. It is a lipid-soluble
beta hydroxy acid that may penetrate sebum-plugged pores. It is available in
concentrations of 0.5% to 2% and is considered second-line treatment.
Salicylic acid is found in many body washes and cleansers, as well as in
topical creams and gels. Generally, the body washes and cleansers are not very
effective, because the contact time on the skin is short. Adverse effects
include transient stinging or burning of the skin, as well as redness or
irritation.
Sulfur and
Sulfur-Resorcinol:
Precipitated or colloidal sulfur is a keratolytic and antibacterial agent
utilized to treat acne in concentrations of 3% to 10%. Sulfur 3% to 8% may be
combined with resorcinol 2% to increase the effect of sulfur. Possible
disadvantages of these products include the noticeable color and odor of
sulfur, as well as the possible dark brown scaling caused by resorcinol on
darker skin (reversible). In addition, these products may be comedogenic when
used consistently and therefore are better utilized for short-term spot
treatment.
Herbal Products:
There are several herbal products that may be effective in treating acne.
Common ingredients in these products include alpha hydroxy acids, such as
glycolic acid; tea tree oil; bovine cartilage; guggul; Saccharomyces
boulardii; and zinc. Glycolic acid, in concentrations of 70%, may be used
in face peels, significantly improving atrophic acne scars, while a
concentration of 15% is moderately effective as a daily lotion or face wash.
When tea tree oil 5% was compared to benzoyl peroxide 5%, it was found to
significantly reduce the number of inflammatory lesions and comedones. Benzoyl
peroxide was statistically superior in reducing the lesions and had a faster
onset of action; however, tea tree oil was associated with fewer side effects.
Tea tree oil may have a place in therapy for patients who are unable to
tolerate the adverse effects of benzoyl peroxide. Oral zinc has been studied
for the treatment of acne, since research has suggested lower serum and skin
zinc levels in patients with acne. Small clinical trials show zinc to be
favorable, but no conclusive data have yet emerged.
Homeopathic formulations
include Acne by Nature's Sunshine, Acne Formula by HERBALmax, and Acne Support
Combo by Traditional Tibetan Healing Inc. These formulations consist of a
combination of various ingredients with insufficient evidence for
effectiveness.14
Role of the Pharmacist
Pharmacists play a
vital role in evaluating the patient. This includes obtaining
medical/medication history, observing the number and types of lesions,
referring patients to a physician if needed, choosing the appropriate
therapeutic regimen, and counseling the patient. To achieve maximal benefit,
patients need to be educated about the goals of treatment, realistic
expectations, length of therapy, appropriate use of products, and the
importance of adhering to the regimen. Many patients may be able to treat
their acne utilizing OTC medications; however, it is imperative that the
pharmacist know which patients to refer to a doctor. Patients should be
referred to a physician if any of the following are noticed:
moderate-to-severe acne (characterized by papules, pustules, cysts, scarring,
nodules), exacerbating factors (e.g., medications), differential diagnosis
(e.g., rosacea, which occurs more often in women and is usually characterized
by papules, pustules, redness on the central portion of the face into the
scalp, and sensitivity to touch and sunlight; onset is usually between ages 20
and 60),15 resistance or allergy to OTC treatment, and
psychological effects.
Conclusion
Acne vulgaris is a
common skin disorder, at times inflicting both physical scarring and
emotional/psychological effects. It is usually self-diagnosed and
self-treated. Although the patient is able to buy many of these products based
on marketing and labeling, the most effective treatment regimens are
individually developed, and include both pharmacologic and nonpharmacologic
measures. At times, OTC treatments may be utilized in conjunction with
prescription products to treat acne. The pharmacist is a great source for
appropriate product selection and educational and empathetic counseling.
References
1. West DP, West LE, Musumeci ML, et al. Acne vulgaris. In: DiPiro JT, Talbert RL, Yee GC, et al., eds. Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York, NY: McGraw-Hill; 2005:1755-1768.
2. Foster KT, Coffey CW. Acne. In: Berardi RR, Kroon LA, McDermott JH, et al, eds. Handbook of Nonprescription Drugs: An Interactive Approach to Self-Care. 15th ed. Washington, DC: American Pharmaceutical Association; 2006:803-816.
3. Ayer J, Burrows N. Acne: more than skin deep. Postgrad Med J. 2006;82:500-506.
4. James WD. Clinical practice. Acne. N Engl J Med. 2005;352:1463-1472.
5. National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Questions & answers about acne. Available at: www.niams.nih.gov/hi/topics/acne/AcneRP.pdf. Accessed December 1, 2006.
6. Leyden JJ. Therapy for acne vulgaris. N Engl J Med. 1997;336:1156-1162.
7. Arndt KA, Bowers KE, eds. Manual of Dermatologic Therapeutics with Essentials of Diagnosis. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2001:3-20.
8. Thiboutot D. New treatments and therapeutic strategies for acne. Arch Fam Med. 2000;9:179-187.
9. Russell JJ. Topical therapy for acne. Am Fam Physician. 2000;61:357-366
10. Tan H. Topical antibacterial treatments for acne vulgaris: comparative review and guide to selection. Am J Clin Dermatol. 2004;5:79-84.
11. Taylor GA, Shalita AR. Benzoyl peroxide-based combination therapies for acne vulgaris. Am J Clin Dermatol . 2004;5:261-265.
12. O'Mara NB. Comparison of antimicrobial treatments for mild to moderate acne. Pharmacist's Letter/Prescriber's Letter. 2005;21:210312.
13. Burkhart CG, Burkhart CN. Treatment of acne vulgaris without antibiotics: tertiary amine-benzoyl peroxide combination vs. benzoyl peroxide alone (Proactiv Solution). Int J Dermatol. 2007:46:89-93.
14. Jelin J. Pharmacist's Letter/Prescriber's Letter. Natural Medicines Comprehensive Database. www.naturaldatabase.com/(S(3mhfsfbnooryus45zyoo3nrf))/nd/Search.aspx?cs=&s=nd&pt=&sh=0&fs=PL&id=977&r=3&searchid=3214225&txt=acne. Accessed January 15, 2007.
15. Purdy S, de Berker D. Acne.
BMJ. 2006;333:949-953.
To comment on this article,
contact editor@uspharmacist.com.





