National Poison Prevention
Week is a yearly event that was established by Congress and President John F.
Kennedy in 1961 through Public Law 87-319.1 Designated in the third
week of March, it is the focus of annual activities intended to prevent
accidental poisonings.
Poison Statistics
The U.S. Consumer
Products Safety Commission issued a warning to coincide with the 2005 Poison
Prevention Week.2 The organization reported that unintentional
poisonings were responsible for over one million calls to poison control
centers and 78,000 hospital visits for children ages younger than 5 years in
2003. The data were compiled by the American Association of Poison Control
Centers and the National Poison Prevention Week Council, as well as the
Consumer Product Safety Commission.
Acetaminophen
Acetaminophen has
been a leading cause of poisoning for many years. It is the most common reason
for poisonings in the United Kingdom, being the source of 50% of acute
poison-related hospital admissions.3 Thus, the U.K. introduced
legislation in 1998 to restrict sales, which may have reduced its dangers.
4 One reason for this problem is a widespread perception of nontoxicity.
An example may prove
instructive. A 17-year-old high school teenager took 20 tablets of 500-mg
acetaminophen over a three-hour period for migraine.5 While
acetaminophen is also a common vehicle for suicide, physicians confirmed that
her intent was not suicidal.6 She began vomiting, and her vital
organs gradually failed. Prior to her death, she regained consciousness long
enough to state, "I'm so sorry, Ma. I didn't realize that I took that many
pills. I thought it was OK. It's just Tylenol, Ma." Pharmacists must stress
the toxicity of acetaminophen products at the point of sale. Alternatively,
they might transfer these products to a location behind the counter to ensure
that patients are properly advised on their dangers.
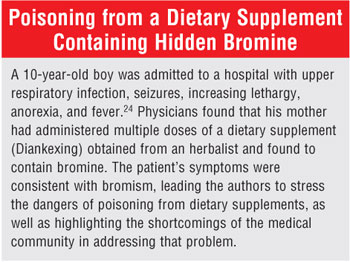
Poisoning Caused by Dietary
Supplements
Few categories of
poisoning are as disappointing and difficult to research as those caused by
dietary supplements. These poisonings are disappointing because dietary
supplements are a group of products whose legal meaning is ill-defined and
whose pharmacology and toxicology are incompletely elucidated due to the lax
strictures inherent in the retrogressive Dietary Supplement Health and
Education Act (DSHEA) of 1994.7 Since manufacturers are not
required to conduct the research needed to prove efficacy or safety, many
simply do not do so. Thus, the average health food store stocks hundreds of
products whose safety profiles are unknown.
Manufacturers have therefore
neglected carrying out the standard toxicological tests, such as those
required of prescription products, because they are not required to do so;
they are also not required to report adverse events to the FDA.7
Furthermore, DSHEA does not require premarketing testing of dietary
supplements for such contaminants as lead, cadmium, or arsenic. Thus, a child
taking an overdose of any herb may also be exposed to unidentified toxins. The
Institute of Medicine further observed that American consumers assume
incorrectly that some governmental agency regulates dietary supplements with
rules similar to those governing legitimate nonprescription products.7
Conium maculatum
Conium
maculatum is the
scientific name for poison hemlock.8,9 An authoritative review
presented various aspects of the herb, including the fact that it was used to
kill Socrates in 399 b.c.8 It contains a variety of piperidine
chemicals known as the coniine alkaloids, also found in aloes. The
chemicals are neurotoxins, with ingestion possibly resulting in nausea and
vomiting, abdominal pain, tachycardia, seizures, ascending paralysis, muscular
tremor, weakness, and coma and death from respiratory failure.8
Unfortunately, herbal and homeopathic companies have marketed products
containing hemlock, usually labeling it Conium maculatum or Succus
conii, which serves to mislead consumers about potential toxicity, as this
practice hides its more commonly understood name. Homeopathic Web sites
recommend it for hundreds of unproven uses, e.g., vertigo, red ear wax,
striped shapes in front of the eyes, corneal ulceration, cancer of the face,
pain in the breast, crusty ulcers on the skin, and "hard" cancers.
10 As a result of a resurgence of interest in these unproven claims, one
can even purchase poison hemlock seeds on the Internet.11 While it
is true that there are no published reports of toxicity or poisoning from
herbal or homeopathics containing poisonous hemlock alkaloids, the Institute
of Medicine pointed out: "Absence of evidence of risk does not indicate that
there is no risk."7
Veratrum album
Veratrum
album has been described
as a "violent irritant poison."12 Two individuals drank
a bitter fluid extract of the roots and experienced nausea, vomiting,
headache, sinus bradycardia, and diarrhea.12 Although they
recovered, the course of more severe poisonings can only be conjectured.
Despite lack of proof of safety and efficacy for any use, it is a popular
homeopathic remedy. It is allegedly effective for nonsense delirium, vertigo,
suppressed urine, gallstone pain, forcible vomiting, black stools, "shrivelled
[sic] fingers," comatose sleep, and hundreds of other unproven uses.
13 Herbalists and others can purchase seeds of this toxic plant on the
Internet.14
Pyrrolizidine Alkaloids
Another danger
arises from herbs that contain pyrrolizidine alkaloids. They include
comfrey--the subject of a 2001 FDA letter to dietary supplement interest
groups. The agency asked them to discontinue the products and to warn
consumers to cease their use immediately.15 The alkaloids are the
cause of hepatic veno-occlusive disease, and several reports of human toxicity
had appeared by 2001. They are also potential carcinogens.15-17
Despite the clear warning regarding toxicity, several firms could be found
selling comfrey on the Internet in 2006. (For safety reasons, their sites will
not be provided.) If asked, pharmacists should advise against ingestion of
comfrey in any form. Having an herb of unproven benefit and suspected or
proven toxicity in the house also exposes children to the dangers of hepatic
failure if it is accidentally ingested in a poisoning episode.
Contaminated Herbal Teas
In 1994, several
cases of toxicity involving an herbal tea known as Paraguay tea were
reported by the Centers for Disease Control and Prevention.18 The
leaves were purchased commercially; three families were affected, and three
individuals required emergency treatment. While the tea was undoubtedly
thought to be safe by those who purchased and brewed it, it nevertheless
contained atropine, scopolamine, and hyoscyamine. A grocer had purchased the
tea directly from farmers, and it apparently had been contaminated by another
plant. This report exposes the dangers inherent in the unrestrained and
unregulated sale and use of herbals. The FDA had warned consumers about
toxicity of herbal teas as early as 1991.19 Their availability
within the home could allow children to eat the raw leaves that are used for
brewing, or to consume the tea itself.
Poisoning Caused by Topical
Pesticides
Lindane was once
considered appropriate therapy for pediculosis (head lice). However, it was
shifted by the FDA to second-line therapy in 1995.20,21 At that
time, because of toxicity issues, the agency limited package sizes, required a
boxed warning, and required the dissemination of a medication guide with each
new prescription. There are an estimated one million prescriptions written for
lindane each year. In 2005, the Centers for Disease Control and Prevention
published a review of unintentional ingestions of topical lindane, spanning
the years from 1998 to 2003.22 The research uncovered 857 cases,
with 8% suffering adverse effects of moderate severity and 1% experiencing
effects of high severity. Signs and symptoms included vomiting (59%), nausea
(18%), oral irritation (19%), and abdominal cramping, cough, and seizure in 3%
to 4% of cases.
Adults mistook lindane for
cough syrup in many cases. In one, a pharmacy misfilled a prescription for
albuterol syrup with lindane. In another, a 47-year-old Texas man ingested 1
ounce of lindane in the mistaken belief it was cough syrup.22 He
experienced vomiting. Also, a 3-year-old boy ingested 1 teaspoonful of 1%
lindane shampoo.22 The mother induced vomiting twice. Despite this,
he collapsed one hour postingestion and experienced a tonic-clonic seizure
that was four to five minutes in duration. He was discharged in stable
condition from the emergency department three hours after admission. Lindane
alternatives for head lice include synergized pyrethrins, permethrin, and
malathion. Those substances were responsible for an additional 523
unintentional poisoning cases during the years included in the study.
The agency concluded that
declining use of lindane will ameliorate the danger somewhat, but pharmacists
should never transfer lindane from its manufacturer-supplied 1- or 2-ounce
bottles into pharmacy bottles that are identical to those used for oral
medications, such as cough syrups. It might be advisable to ensure that
lindane and other pesticides are not in the house to prevent causing
accidental ingestion.20 The pharmacist can aid in this effort by
educating physicians and consumers about nontoxic, environmentally safe
alternatives to pediculosis, like thorough combing with specially designed
combs that remove live lice and nits.
Pyridoxine
Pyridoxine is
thought to be useful in treating such problems as premenstrual syndrome. This
is an unproven claim, but women who take this product and keep it in their
homes may also have children who could gain access to it. Overdoses may result
in ataxia, incoordination, and seizures.23 Like other potentially
dangerous substances, it should be kept away from children.

REFERENCES
1. National Poison Prevention
Week. Available at: poisonprevention.org/ faq.html#6. Accessed January 17,
2006.
2. News from Consumer Product Safety
Commission. Press release #05-136. March 15, 2005.
3. Greene SL, Dargan PI, Jones AL.
Acute poisoning: Understanding 90% of cases in a nutshell. Postgrad Med J
. 2005;81:204-216.
4. Morgan O, Majeed A. Restricting
paracetamol in the United Kingdom to reduce poisoning: a systematic review.
J Public Health. 2005;27:12-18.
5. Killackey J. Teen's death shows
danger of overdosing on over-the-counter pills. Daily Oklahoman. July
2, 2003;1-A, 2-A.
6. Farley A, Hendry C, Napier P.
Paracetamol poisoning: physiological aspects and management strategies.
Nurs Stand. 2005;19:58-64.
7. Institute of Medicine and National
Research Council. Dietary Supplements: A Framework for Evaluating Safety.
National Academy Press: Washington, D.C.; 2004.
8. Reynolds T. Hemlock alkaloids from
Socrates to poison aloes. Phytochemistry. 2005;66:1399-1406.
9. Brooks DE. Plant poisoning,
hemlock. Available at: www.emedicine.com/emerg/topic875.htm. Accessed January
17, 2006.
10. Conium maculatum.
Available at: www.abchomeopathy.com/r.php/Con. Accessed January 17, 2006.
11. HerbalFire.com Products:
Conium maculatum poison hemlock, hemlock seeds for sale. Available at: www.
herbalfire.com/poison_hemlock.htm. Accessed January 17, 2006.
12. Zagler B, Zelger A, Salvatore C,
et al. Dietary poisoning Veratrum album: a report of two cases. Wien
Klin Wochenschr. 2005;117:106-108.
13. Veratrum album. Available
at: www.abchomeopathy.com/r.php/Verat. Accessed January 17, 2006.
14. Chiltern seeds. Available at:
www.edirectory.co.uk/chilternseeds/pages/default.asp?recordid=BIECH&cid=211.
Accessed January 17, 2006.
15. FDA advises dietary supplement
manufacturers to remove comfrey products from the market. Available at:
cfsan.fda.gov/~dms/dspltr06.html. Accessed January 17, 2006.
16. Pyrrolizidine alkaloids.
Available at: www.cfsan.fda.gov/~mow/chap42.html. Accessed January 17, 2006.
17. Chaparral-induced toxic
hepatitis--California and Texas, 1992. Available at: www.cdc.gov/mmwr/preview/
mmwrhtml/00017883.htm. Accessed January 17, 2006.
18. Anticholinergic poisoning
associated with an herbal tea--New York City, 1994. Available at: www.cdc.gov/
mmwr/preview/mmwrhtml/00036554.htm. Accessed January 17, 2006.
19. Snider S. Beware the unknown
brew: herbal teas and toxicity. FDA Consumer. 1991;25:30-33.
20. FDA issues health advisory
regarding labeling changes for lindane products. Available at: www.fda.gov/bbs/
topics/ANSWERS/2003/ANS01205.html. Accessed January 17, 2006.
21. FDA public health advisory:
safety of topical lindane products for the treatment of scabies and lice.
Available at: www.fda.gov/cder/drug/infopage/lindane/lindanePHA.htm. Accessed
January 17, 2006.
22. Unintentional topical lindane
ingestions--United States, 1998–2003. Available at: www.cdc.gov/mmwr/
preview/mmwrhtml/mm5421a2.htm. Accessed January 17, 2006.
23. Lheureux P, Penaloza A, Gris M.
Pyridoxine in clinical toxicology: a review. Eur J Emerg Med.
2005;12:78-85.
24. Boyer EW, Kearney S, Shannon MW,
et al. Poisoning from a dietary supplement administered during
hospitalization. Pediatrics. 2002;109:E49.
To comment on this article,
contact
editor@uspharmacist.com.






