US Pharm.
2006;7:53-57.
Sleep
apnea is very common--an estimated 12 million Americans have been diagnosed
with the condition. Because sleep apnea frequently goes undiagnosed, many
experts agree that millions more Americans could have the condition.1-3
In general, sleep apnea occurs more often in males than females
(approximately 24% of males and 9% of females have sleep apnea) and in adults
older than 40 years. However, anyone can have sleep apnea, regardless of age.
1,3 Because patients with sleep apnea have a high risk of morbidity and
mortality, it is important that educational materials regarding the condition
be made available to help them better understand and manage their diagnosis.
3,4 This patient-focused article was designed to assist pharmacists in
counseling patients on sleep apnea.
What Is Sleep Apnea?
Sleep apnea is a
serious disorder in which people stop breathing repeatedly during sleep. These
gaps in breathing--known as apneas--usually last at least 10 seconds and
are commonly accompanied by snoring, especially in obstructive sleep apnea.
2 (The Greek word apneameans without breath.)1 Sleep apnea
can disrupt sleep-wake cycles and prevent patients from getting restful sleep.
Consequently, people suffering from sleep apnea frequently complain of daytime
sleepiness.3
What Are the Types of Sleep
Apnea?
Sleep apnea can be
categorized into three types: obstructive, central, and mixed.1-8
In all three, people with untreated sleep apnea stop breathing repeatedly
during their sleep, sometimes hundreds of times during the night and often for
a minute or longer.2
Obstructive Sleep Apnea:
The most common form of sleep apnea, obstructive sleep apnea is characterized
by snoring. However, not everyone who snores has obstructive sleep apnea--only
one in four heavy snorers has the condition.3 Obstructive sleep
apnea occurs when tissues in the upper airway completely or partially collapse
at intervals during sleep and block the passage of air.3,6 These
apneic events decrease the amount of oxygen in the blood, and this lack of
oxygen eventually triggers the lungs to suck in air. This causes patients to
gasp or snort but does not usually fully wake them. In most cases, people with
obstructive sleep apnea are not aware that they have the condition. Not
surprisingly, symptoms are most frequently reported by bed partners.3
Only in rare circumstances does obstructive sleep apnea cause patients to
totally wake from sleep. However, because sleep-wake cycles are disturbed,
patients who have obstructive sleep apnea commonly complain of daytime
sleepiness, which can adversely affect their quality of life.3,6
Furthermore, patients with obstructive sleep apnea are more likely to suffer
sleep-related motor vehicle accidents, hypertension and other serious
cardiovascular complications, and increased mortality and morbidity.8
The most common risk factors
of obstructive sleep apnea include obesity; polyps in the upper airway; and
enlarged tonsils, adenoids, and/or tongue. Additionally, conditions such as
acromegaly, amyloidosis, and hypothyroidism, as well as neurologic conditions
that impair upper airway muscle tone, can cause obstructive sleep apnea.3
Central Sleep Apnea:
Much less common than obstructive sleep apnea, this form of sleep apnea
accounts for about only 10% of sleep apnea cases.3 In central sleep
apnea, the respiratory drive is impaired because the brain fails to signal the
respiratory muscles to breathe. When this occurs, oxygen levels drop abruptly,
causing the affected person to wake suddenly and gasp for air. In contrast to
those with obstructive sleep apnea, people with central sleep apnea usually
recall waking after apneic episodes. Additionally, patients with central sleep
apnea typically experience less daytime sleepiness than do those with
obstructive sleep apnea.1,3,5
Central sleep apnea usually
occurs in patients who have experienced some form of central nervous system
insult (e.g., a stroke or a neuromuscular disease such as amyotrophic lateral
sclerosis or encephalitis). This apnea has also been reported in patients who
have heart failure and other cardiac and pulmonary diseases.
Mixed Sleep Apnea:
Some patients have both obstructive and central sleep apnea. It is not
uncommon for patients with mixed sleep apnea to exhibit both forms of apnea in
the same apneic episode. In addition, patients can have a mix of central,
mixed, and obstructive apneas in the same night. Mixed sleep apnea is found
most commonly in infants and young children who have abnormal breathing
control.7
What Are the Symptoms of
Sleep Apnea?
Many people with obstructive sleep
apnea complain that they wake up with an extremely sore and/or dry throat or
that they have woken with a choking or gasping sensation. Patients may even
admit to waking themselves with their own snoring. Many patients with
obstructive sleep apnea are extremely tired during the day because of
sleep-wake cycle disruptions. Additional symptoms include morning headaches,
forgetfulness, depressed mood, and decreased interest in pleasurable
activities (e.g., sex).3,6
Unlike patients with
obstructive sleep apnea, patients with central sleep apnea often have trouble
falling and staying asleep. It is not uncommon for patients with central sleep
apnea to also experience a choking or gasping sensation upon awakening.3
What Are the Risk Factors
for Sleep Apnea?
Risk factors for
sleep apnea include a family history of sleep apnea; obesity; male gender;
large neck; recessed chin; structural abnormalities in the upper airway;
African-American, Pacific Islander, or Mexican descent; smoking; and alcohol
use. In addition, the prevalence of certain medical conditions (e.g.,
diabetes, gastroesophageal reflux disease, hypothyroidism, polycystic ovarian
syndrome, chronic upper airway conditions) seem to predispose patients to
developing sleep apnea. Despite these risk factors, sleep apnea can affect men
and women of all ages and weights, including young children and infants.
1,5,9,10
Certain medications can worsen
sleep apnea. Therefore, patients with sleep apnea should be encouraged to
avoid all central nervous system depressants, including alcohol, anxiolytics,
antihistamines, hypnotics, and narcotics.3,5
What Are the Consequences
of Untreated Sleep Apnea?
The consequences of untreated sleep
apnea can be extremely dangerous--even deadly. Sleep apnea is associated with
cardiovascular problems such as high blood pressure, cardiac arrhythmias,
pulmonary hypertension, heart failure, heart attacks, and stroke.2,4,5,11
In addition, patients may fall asleep at inappropriate times and/or
experience morning headaches, memory problems, feelings of depression,
gastroesophageal reflux, the need to use the bathroom frequently at night, and
impotence. Children with untreated sleep apnea are commonly hyperactive.
Finally, untreated sleep apnea can lead to job loss (due to nonproduction),
poor academic performance, and motor vehicle accidents.2
How Is Sleep Apnea
Diagnosed?
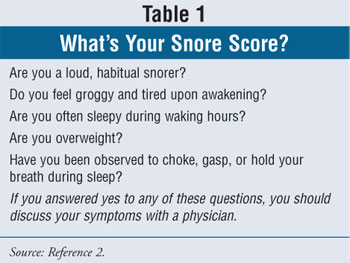
Patients concerned about sleep apnea
are encouraged to compute their Snore Score (Table 1). Those who answer
yes to any of the questions on the Snore Score should discuss their symptoms
with a physician.2
To determine whether a patient
may have sleep apnea, a complete history and physical examination is
necessary. Patients should be assessed for abnormalities in the soft palate or
upper airways, upper body obesity, and wide neck measurements. If sleep apnea
is suspected, a sleep study, or polysomnography, should be considered,
especially in patients who have serious medical conditions that could be
worsened or caused by sleep apnea (e.g., heart disease, high blood pressure,
heart failure, diabetes, chronic headaches, epilepsy, obstructive lung
disease, severe acid reflux) or those who experience decreased quality of life
or increased risk of accidents secondary to the sleep apnea.
Sleep studies--assessments of
brain activity, eye movements, muscle activity, heart rate, respiratory
effort, airflow, and blood oxygen performed during an overnight stay at a
sleep center--are considered the gold standard for diagnosing sleep apnea.
7 However, the tests can be expensive and are not always covered by
insurance. For this reason, individuals who have no health risk factors and no
impairment of quality of life or increased risk for accidents do not typically
require sleep studies.8
How Is Sleep Apnea Treated?
It is imperative
that patients who have been diagnosed with sleep apnea seek treatment, as
untreated sleep apnea can negatively affect health. It may increase the risk
of high blood pressure, heart attack, and sudden death. On the other hand,
effective treatment of sleep apnea may decrease fatigue, improve sleep
quality, decrease blood pressure in patients with hypertension, and lead to
weight loss in obese patients.8 Treatment of sleep apnea must be
individualized and depends upon the severity of the apneic spells and the
amount of sleep disruption.3
In general, there are four
categories of sleep apnea treatment: (1) lifestyle changes, (2) drug therapy,
(3) devices, and (4) surgical interventions.3,8-10,12
Lifestyle Changes:
For patients with mild obstructive sleep apnea, lifestyle changes may
alleviate the condition.8 Overweight patients are encouraged to
lose weight--a 10% weight loss can reduce the number of apneic events for most
patients.5 Patients should be encouraged to avoid agents such as
alcohol, antihistamines, sedatives, and hypnotics that make the airway more
likely to collapse during sleep and prolong apneic periods.3,5
Additionally, changing sleep positions (from supine to lateral) may promote
regular breathing in patients who have at least twice as many respiratory
events in supine positions compared with lateral positions. Tennis balls
attached to the pajamas or wedge pillows may be used to train patients to
sleep in lateral positions.10 Finally, remind patients of the
importance of adopting good sleep habits. Tell them to keep their bedroom
cool, quiet, comfortable, and free of unnecessary light; to go to bed at the
same time each night; to get up at the same time each morning; and to avoid
using a computer or watching television in bed.13
Drug Therapy:
For the most part, drug therapy has not demonstrated much benefit in the
treatment of sleep apnea. In general, medications should be reserved for
patients with mild disease or who resist lifestyle changes. Antidepressant
medications, such as protriptyline and fluoxetine, have shown only minimal
promise in patients with obstructive sleep apnea. In theory, these products
reduce the frequency of apneas and increase oxygen saturation.3,10
Acetazolamide may be useful for some patients with central sleep apnea,
because it induces a metabolic acidosis that stimulates respiratory drive.
3,10,14
However, using medications to
treat accompanying disorders that may be associated with sleep apnea may be
beneficial. Thyroid hormone replacement therapy may decrease apneic episodes
in patients suffering from hypothyroidism. Theophylline has shown promise in
treating central sleep apnea in patients who also have heart failure. Proton
pump inhibitors may decrease apneic episodes in patients with severe acid
reflux.3
Devices:
Devices that provide continuous positive airway pressure (CPAP) during sleep
are considered the treatment of choice for all types of sleep apnea, according
to guidelines from the American Academy of Sleep Medicine.3,5,12
(Of note, for patients suffering from central sleep apnea, CPAP is typically
used along with supplemental oxygen.3) CPAP therapy involves having
the patient sleep with a nose or face mask connected to a mechanical device
that delivers air or oxygen to the patient's nose throughout the night at a
constant pressure that is greater than atmospheric pressure. The increased
pressure is transferred to the pharynx, where it acts as a pneumatic splint to
prevent the airway from collapsing. CPAP therapy is relatively noninvasive and
often associated with a rapid response.4 Compliance--ranging from
25% to 70%--can be a major limitation with CPAP.3 Many people
feel like they are suffocating when they use CPAP and complain of nasal
dryness, intestinal gas, and conjunctivitis.5 Additionally, CPAP is
expensive (costs of CPAP devices range from $700 to $1,000), and some of the
equipment is bulky and noisy, is not easily portable, and requires electricity.
5,12 Regardless, pharmacists should encourage patients to be compliant
with CPAP, because one night of noncompliance results in a complete reversal
of the gains made in daytime altertness.3
More recently, bilevel
positive airway pressure (BiPAP) has been used to treat sleep apnea. BiPAP
uses an electronic circuit to monitor breathing and provides two different
pressures, a higher one during inhalation and a lower pressure during
exhalation. BiPAP is expensive, costing two to three times more than CPAP, but
allows for improved patient comfort in those who require higher than average
CPAP pressures and/or find breathing against increased pressure to be
uncomfortable or disruptive to their sleep.10
Mandibular repositioning
devices can also be used to treat obstructive sleep apnea.5,12
These devices decrease apnea by advancing the mandible 5 to 6 mm forward,
moving the tongue base anteriorly and allowing for better breathing. Because
these devices are less effective than CPAP in reducing apneic episodes, the
American Sleep Disorders Association recommends them only for patients who
cannot tolerate CPAP.12
Surgical Interventions:
Surgical interventions may be necessary for patients with obstructive sleep
apnea who continue to have impairment despite CPAP, behavioral modifications,
and drug therapy. Such procedures are designed to bypass the obstruction or to
prevent collapse of the tissue at the site of obstruction. Surgical options
include uvulopalatopharyngoplasty (removal of a rim of the soft palate and the
uvula), tonsillectomy (removal of the tonsils), nasal surgery (removal of
nasal obstructions), and maxillomandibular advancement surgery (jaw surgery).
However, few randomized clinical trials have been conducted to verify the
long-term efficacy of these procedures.3,4,5,12,15
Tracheotomy is the only
surgical procedure known to cure patients with severe obstructive sleep apnea.
The placement of a tracheotomy tube or the creation of a more permanent
skin-lined tracheotomy often results in profound symptom improvements.
However, only patients with life-threatening, severe obstructive sleep apnea
should have this surgery, since many risks and complications (e.g., formation
of scar tissue at the opening, difficulty speaking, bleeding and infection at
the site, and increased risk of lung infections) can occur as a result of the
procedure.12,15
Conclusion
Sleep apnea is
neither an uncommon nor benign condition. Sleep apnea can affect the very
young, the very old, and everyone in between. In addition, sleep apnea can
have devastating consequences--patients are more prone to accidents and other
serious health conditions. Fortunately, good treatments exist, and pharmacists
are available to educate patients about preventing and treating this common,
but often undiagnosed, medical condition.
References
1. National
Institutes of Health. What Is Sleep Apnea? Available from:
www.nhlbi.nih.gov/health/dci/Diseases/SleepApnea/SleepApnea_WhatIs.html.
Accessed June 2006.
2. American Sleep Apnea
Association. Tired of the Sleepiness? Available from:
www.sleepapnea.org/resources/brochure.html. Accessed November 2005.
3. Jackson CW, Curtis
JL. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A
Pathophysiological Approach. 6th ed. New York, NY: McGraw-Hill;
2005:1326-1327.
4. Dincer HE, O'Neill
W. Deleterious effects of sleep-disordered breathing on the heart and vascular
system. Respiration. 2006;73:124-130.
5. Williams DM, Kradjan
WA. In: Koda-Kimble MA, Young LY, Kradjan WA, et al, eds. Applied
Therapeutics: The Clinical Use of Drugs. 8th ed. Vancouver, WA: Lippincott
Williams & Wilkins. 2005:24-24 to 24-25.
6. Stierer T, Punjabi
NM. Demographics and diagnosis of obstructive sleep apnea. Anesthesiol Clin
North America. 2005;23:405-420.
7. Strohl KP. In: Arend
WP, Armitage JO, Drazen JM, et al, eds. Cecil Textbook of Medicine.
22nd ed. Philadelphia, PA: W. B. Saunders Company 2004:576-580.
8. Czeisler CA,
Winkelman, JW, Richardson GS, Phillipson EA. In: Braunwald E, Fauci AS, Kasper
DL, et al, eds. Harrison's Principles of Internal Medicine. 15th
ed. New York, New York: McGraw Hill; 2001;161: 1520-1523.
9. Rock P. Obesity and
sleep apnea. Anesthesiol Clin North America. 2005;23:xiii-xv.
10. Magalang UJ, Mador
MJ. Behavioral and pharmacological therapy of obstructive sleep apnea. Clin
Chest Med. 2003;24:343-353.
11. Yaggi H, Mohsenin
V. Obstructive sleep apnoea and stroke. Lancet Neurol. 2004;3:333-342.
12. Couch ME, Senior B.
Nonsurgical and surgical treatments for sleep apnea. Anesthesiol Clin North
America. 2005;23:525-534.
13. National Institutes
of Health. Lifestyle Changes. Available from:
www.nhlbi.nih.gov/health/dci/Diseases/nar/nar_treatments.html. Accessed June
2006.
14. Javaheri S.
Acetazolamide improves central sleep apnea in heart failure. Am J Respir
Crit Care Med. 2006;173:234-237.
15. Victor LD.
Treatment of obstructive sleep apnea in primary care. Am Fam Physician.
2004;69:561-568.
16. Erenberg A, Leff
RD, et al. Caffeine citrate for the treatment of apnea of prematurity: a
double-blind, placebo-controlled study. Pharmacotherapy.
2000;20:644-652.
17. Halbower AC, Marcus
CL. Sleep disorders in children. Curr Opin Pulm Med. 2003;9:471-476.
To comment on this article, contact
editor@uspharmacist.com.






