US Pharm. 2006;12:32-48.
The estimated worldwide prevalence of subclinical hypothyroidism, based on previous population studies, is about 7.5% to 8.5% in women and 2.8% to 4.4 % in men.1,2 The age-dependent increase in rates of subclinical hypothyroidism is higher in women than in men, with near equal rates between genders around the mid-70's. An approximate 20% prevalence was seen in women older than 60.1,2 In the United States, the prevalence of this condition is lower in African Americans than in Caucasians. 3
Subclinical hypothyroidism is more common in patients with type 1 diabetes and those with a history of neck irradiation and postpartum thyroiditis.4,5 Approximately 2% of pregnant women have subclinical hypothyroidism, primarily with elevated serum antithyroid antibody concentrations.6 Patients who have autoimmune thyroid disease or who have received radioiodine therapy or high-dose external radiotherapy are likely to progress to overt hypothyroidism. In contrast, subclinical hypothyroidism is likely to persist in those who have had thyroid surgery for indications other than hyperthyroidism or in those who have received external radiotherapy during childhood. In Europe, where iodine intake is variable, subclinical hypothyroidism is more prevalent in areas of iodine sufficiency. The prevalence of subclinical hypothyroidism is estimated to be 4.2% in iodine-deficient areas and 23.9% in areas of iodine intake, despite a similar incidence of patients with high serum concentrations of antithyroid peroxidase antibodies.7
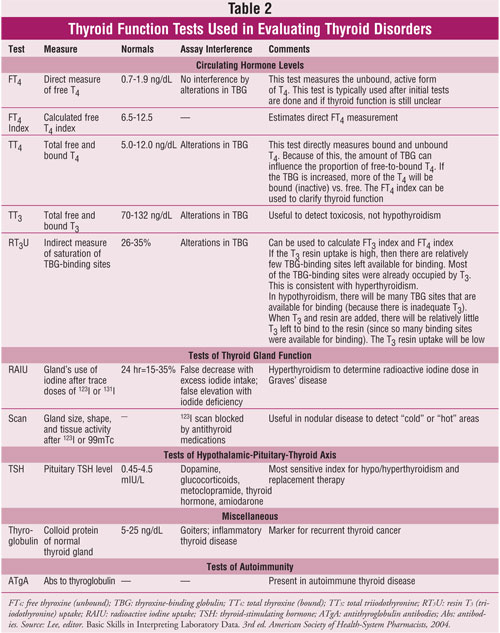
Thyroid-stimulating hormone (TSH) is a sensitive and specific measure of thyroid function. In this case scenario, unlike patients with overt hypothyroidism, elevations in TSH may not be present with normal free thyroxine (T4) and triiodothyronine (T3) concentrations. Figure 1 and Tables 1 and 2 provide an algorithm for a thyroid panel to determine thyroid dysfunction and description of laboratory indices necessary to assist in diagnosis of thyroid failure. These aforementioned objective findings are referred to as subclinical hypothyroidism,even though patients may have early clinically subjective symptoms. A differential diagnosis leading to thyroid disease may be missed, since early clinical symptoms, such as constipation and fatigue, may be attributed to aging.

An expert panel representing the American Thyroid Association, American Association of Clinical Endocrinologists, and The Endocrine Society convened in 2002 helped to further refine the definition of subclinical hypothyroidism regarding reference ranges for serum TSH, based on a series of studies.8,9 The panel defined the reference range for TSH as 0.45 to 4.5 mIU/mL, and subclinical hypothyroidism was defined as serum TSH more than 4.5 mIU/L with normal T3 and T4 values in the presence or absence of symptoms.8

Clinical manifestations, if present, can be explained by assuming that a T4 level of ?6 mcg/dL may represent a significant drop from an original level of 9 or 10 mcg (normal range is 4.5 to 12.5 mcg).10
The etiologies of subclinical and overt hypothyroidism are identical. Chronic autoimmune thyroiditis (Hashimoto's disease) accounts for the majority of cases. Approximately 54% of patients with subclinical hypothyroidism have Hashimoto's disease with high serum concentrations of antithyroid microsomal or antithyroid peroxidase antibodies. 9 Hamburger et al. also observed that patients receiving prior ablative therapy for hyperthyroidism caused by Graves' disease account for approximately 40% of subclinical hypothyroidism cases.9 Other etiologies of subclinical hypothyroidism include early pituitary and hypothalamic disorder, suboptimal levothyroxine replacement therapy in patients with known hypothyroidism, and drug-induced causes with medications, such as amiodarone, lithium, glucocorticoids, dobutamine, and dopamine.11 Sawin et al. determined that 37% of subclinical hypothyroidism cases resulted from patients receiving inadequate T4 replacement therapy for overt hypothyroidism.12
The progression to overt hypothyroidism can occur in approximately 5% of the population per year when detectable antibodies and elevated TSH levels are present.13 In the elderly, the risk is increased to approximately 20%. Differential diagnoses that must be excluded are chronic renal failure, primary adrenal failure, and mutations, resulting in thyrotropin-receptor inactivation.5 Spontaneous recovery has also been seen in patients with subclinical hypothyroidism (silent thyroiditis), although the frequency of this phenomenon is unclear.14-16 Subclinical hypothyroidism is a disorder that has created therapeutic debate over when to screen patients and whether or not to initiate pharmacotherapy. 13
Clinical Manifestations
Common clinical symptomatology
reported with subclinical hypothyroidism includes neuromuscular symptoms
(e.g., weakness, fatigue, paresthesia, cramps) and weight gain. (One study
reported that serum TSH concentrations greater than 3.6 mIU/L and a normal
free T4 were associated with modest weight gain when compared to
those with serum TSH 0.4 to 0.99 mIU/L.)17 Additional symptoms
include hyperprolactinemia and elevated intraocular pressure, both of which
respond to T4 therapy.18,19 Complications associated
with untreated subclinical hypothyroidism are cardiovascular and neuro!=
psychiatric in nature.
The reported cardiovascular manifestations are reflected by cholesterol abnormalities and cardiovascular changes. The evidence regarding elevated cholesterol levels has been conflicting. Most of the research has been derived through cross-sectional studies. Evidence shows that elevations in total cholesterol and LDL cholesterol levels are observed at serum TSH levels more than 10 mIU/L. The Colorado thyroid disease prevalence study, a cross-sectional study involving 25,862 patients, revealed statistically significant elevations in mean total cholesterol in patients with serum TSH between 5.1 and 10 mIU/L vs. euthyroid patients (223 mg/dL vs. 216 mg/dL; P <.03).2 Whether these results are clinically significant in terms of atherosclerotic progression and eventual cardiovascular abnormalities is debatable. Other than this study, however, the majority of cross-sectional analyses have revealed mild to insignificant changes in all lipid parameters.20ñ25 A recent meta-analysis of 247 patients in 13 subclinical hypothyroidism trials revealed that T4 therapy resulted in significant reductions in serum total cholesterol (8 mg/dL [0.2 mmol/L]) and serum LDL cholesterol (10 mg/dL [0.3 mmol/L]); the mean serum HDL cholesterol and triglyceride concentrations did not change. 26 It is important to note that reductions in serum cholesterol were seen only in patients with levels more than 240 mg/dL at baseline. Only those patients who had "subclinical hypothyroidism" based on inadequately treated overt hypothyroidism had statistically significant decreases in serum cholesterol. Luboshitzky et al. conducted a randomized clinical trial studying changes in the blood pressure, body mass index, levels of TSH and free T4 , thyroid antibodies, and lipid panel in 57 women with subclinical hypothyroidism and 34 euthyroid women. Results revealed that women with subclinical hypothyroidism had a higher incidence of diastolic hypertension and elevated lipid panel parameters.27 Thus, it may be argued that more significant changes in lipid profiles may occur in patients that are closest to the overt hypothyroidism end of the continuum.
The cardiovascular changes that occur in subclinical hypothyroidism are considered a progression on the scale that leads to overt hypothyroidism. Several studies have shown that subclinical hypothyroidism is associated with cardiovascular disease, coronary heart disease (CHD), and all-cause mortality.28ñ34 The changes in cardiac function associated with subclinical hypothyroidism are centered on alterations in diastolic dysfunction, cardiac output reductions, peripheral vascular resistance elevations, increases in carotid intima media-thickness, and left ventricular ejection fraction elevations during periods of maximal exercise.35ñ39 Elevations in proinflammatory markers observed with subclinical hypothyroidism include C-reactive protein, plasma asymmetric dimethylarginine (an endogenous nitric oxide synthase inhibitor), and platelet-aggregating factor.34,40 These markers may contribute to the development of lipid abnormalities and CHD. A recent meta-analysis of 14 observational studies of 13,011 patients diagnosed with subclinical hypothyroidism, with TSH cutoffs ranging from >2.8 to >6.0 mIU/L, confirmed a significant association between the disorder and CHD risk.41 The analysis also underscored the necessity of clinical trials in assessing the potential role of T4 therapy in CHD risk reduction.
Neuropsychiatric manifestations include depression, anxiety, bipolar affective and panic disorders, dementia, and poor psychometric test scoring. Confounding variables, such as concomitant lithium use, inadequate control groups, and the presence of antithyroid microsomal antibodies, have made the assessment of neuro!= psychiatric manifestations of subclinical hypothyroidism difficult. Nevertheless, several studies have shown an increased prevalence of depression and panic disorder and a higher lifetime frequency of depression vs. euthyroid patients.42-44 Monzani et al. demonstrated that women with subclinical hypothyroidism who presented to a clinic for goiter assessment had increased rates of anxiety, hysteria, abnormal psychometric testing, and somatic and depressive manifestations, compared to euthyroid patients with goiter.45 These manifestations were reduced with T4 therapy.
Pregnancy
Available literature analyzing
the role of subclinical hypothyroidism in producing adverse outcomes in
pregnancy has only shown a moderate association. Haddow et al. assessed the
correlation between maternal thyroid deficiency and pediatric neuropsychiatric
development. Sixty-two children whose mothers had high serum TSH (48 of whom
were not treated) and low serum T4 concentrations during the second
trimester were compared with 124 children of mothers whose serum TSH
concentrations were normal.46 At ages 7 to 9, the children with
abnormal TSH values had slightly lower IQ scores than the children with normal
TSH† values (IQ score 103 vs. 107; P = .06). Furthermore, 15% of
the abnormal TSH group but only 5% of the normal group had scores of 85 or
lower. Based on this trial, the clinical significance remains unknown and
warrants future randomized clinical trials. However, undetected subclinical
hypothyroidism in pregnancy remains a potential risk factor for poor
developmental outcomes in offspring. If untreated, even mild hypothyroidism
can lead to severe mental and growth retardation. Development may be delayed
early on, as demonstrated by the failure to meet early milestones. For this
reason, the consensus panel recommends gestational TSH screening in women at
elevated risk whether they are pregnant or plan to become pregnant.8
Women at elevated risk include those with a family or past medical history of
thyroid disease, symptoms of hypothyroidism, type 1 diabetes, goiter, or an
autoimmune disorder.
Screening and Management
Recommendations regarding when to
routinely screen patients have been inconsistent (see Table 3). The
U.S. Preventative Services Task Force does not support screening in
asymptomatic adults. Helfand et al. recommend screening in females older than
40 years or those who reside in geriatric facilities.47 In absence
of definitive guidance, clinicians may elect to screen serum TSH routinely or
reserve assessment in patients with persistent complaints and risk factors for
thyroid failure.10

One key area of contention regarding subclinical hypothyroidism is whether the benefits of treatment with thyroid hormone outweighs the risks. The rationales behind the benefits of therapy are threefold. First, therapy may prevent the progression to overt hypothyroidism. Second, therapy may reverse the cognitive and psychiatric abnormalities associated with the condition. Finally, T4 therapy may delay the progression of cardiovascular disease associated with the progression to overt hypothyroidism. Clinical trials suggest additional benefits from treatment. These benefits included, but were not limited to, reduction in reported symptoms of dry skin, lethargy, cold intolerance, serum lipid concentrations, and cognitive impairments.48-55 It is important to note that in two of these studies, no benefit was observed in patients with serum TSH levels less than 10 mIU/L.
The argument against treatment is also threefold, centering on the cost of therapy, the lifelong commitment to a daily medication regimen in asymptomatic patients, and significantly, the danger of overtreatment. Specifically, the Colorado thyroid disease prevalence study determined an overtreatment prevalence of 21%, predisposing the patient to iatrogenic hyperthyroidism and its subsequent complications (e.g., exacerbation of atrial fibrillation and angina pectoris episodes in susceptible patients, osteopenia).2,56
The patient introduced in this article presented with clinical manifestations of mild thyroid failure, as evidenced by decreased energy, inability to concentrate, mood changes, thinning hair, headaches, consistent weight loss plateau, constipation, and fatigability. Lipid markers, although not accessed, would likely be marked but less consistent. However, this pattern and concurrent hypertension increase the patient's risk of cardiovascular disease. Literature has shown evidence of LDL reduction in response to thyroid replacement with levothyroxine.13 It is advisable to watch the TSH level in absence of thyroid replacement in those patients with established cardiovascular disease due to cardiac risk factors associated with thyroid replacement.13
LF had a TSH level of 9 mIU/L and clinical symptoms in absence of elevated thyroid antibodies (not accessed). The treatment of choice is synonymous to therapy for overt hypothyroidism: levothyroxine. Table 4 lists the available thyroid preparations used in the treatment of thyroid disorders. Patients with overt hypothyroidism receive replacement ranging from 75 to 125 mcg or 50 to 100 mcg in the elderly (1.6 mcg/kg/day).10,13 In overt hypothyroidism, levothyroxine is initiated at 25 to 50 mcg daily and titrated in increments of 25 to 50 mcg in approximately six weeks, when steady state is reached. Patients with cardiac disease will be initiated more conservatively at 25 mcg and titrated by 12.5 to 25 mcg in six-week intervals. In comparison, patients with subclinical hypothyroidism can be controlled with 25 to 50 mcg daily. Once control of TSH is achieved (normal range), monitoring of TSH can be altered to every six to 12 months.10,13

Levothyroxine is generally considered first line because of consistent potency, lack of antigenicity, natural replacement of T 4, and prolonged duration of action (once-daily dosing), as well as chemical stability.
LF was initiated on 25 mcg of levothyroxine daily with repeat TSH evaluation six weeks after initiation. TSH levels normalized with repeat analysis, as well as symptom resolution of chief complaint. The presence of elevated thyroid peroxidase antibodies and thyroid function panel (?TSH, ÿ±T4) will likely progress to overt hypothyroidism, warranting candidacy for thyroid replacement. The preponderance of patients with subclinical hypothyroidism will be evaluated on an individualized basis with clinician predilection and direction from evidence-based guideline recommendations.10,13
References
1. Tunbridge WM, Evered DC, Hall
R, et al. The spectrum of thyroid disease in a community: the Whickham survey.
Clin Endocrinol. (Oxf) 1977;7:481.
2. Canaris GJ, Manowitz NR, Mayor GM,
et al. The Colorado thyroid disease prevalence study. Arch Intern Med.
2000;160:526-534.
3. Kanaya AM, Harris F, Volpato S, et
al. Association between thyroid dysfunction and total cholesterol level in an
older biracial population: the health, aging and body composition study.
Arch Intern Med. 2002;162:773.
4. Gray RS, Borsey DQ, Seth J, et al.
Prevalence of subclinical thyroid failure in insulin-dependent diabetes. J
Clin Endocrinol Metab. 1980;50:1034.
5. Cooper DS. Subclinical
Hypothyroidism. N Engl J Med 2001;345:260-265.
6. Klein RZ, Haddow JE, Faix JD, et
al. Prevalence of thyroid deficiency in pregnant women. Clin Endocrinol.
(Oxf) 1991;35:41.
7. Szabolcs I, Podoba J, Feldkamp J,
et al. Comparative screening for thyroid disorders in old age in areas of
iodine deficiency, long term iodine prophylaxis and abundant iodine intake.
Clin Endocrinol. 1997;47:87.
8. Gharib H, Tuttle RM, Baskin HJ, et
al. Consensus Statement: Subclinical Thyroid Dysfunction: A Joint Statement on
Management from the American Association of Clinical Endocrinologists, the
American Thyroid Association, and The Endocrine Society. J Clin Endocrinol
Metab. 2005;90:
9. Hamburger JI, Meier DA, Szpunar
WE. Factitious elevation of thyrotropin in euthyroid patients [letter]. N
Engl J Med. 1985;313:267.
10. Hueston WJ. Treatment of
hypothyroidism. Am Family Phys. 2001;64:1717-1724.
11. Surks MI, Ortiz E, Daniels GH, et
al. Subclinical thyroid disease: scientific review and guidelines for
diagnosis and management. JAMA. 2004;291:228-238.
12. Sawin CT, Geller A, Hershman JM,
et al. The aging thyroid. The use of thyroid hormone in older persons. JAMA.
1989;261:2653.
13. Adlin V. Subclinical
hypothyroidism: deciding when to treat. Am Family Phys.
1998;57:776-780.
14. Huber G, Staub JJ, Meier C, et
al. Prospective study of the spontaneous course of subclinical hypothyroidism:
prognostic value of thyrotropin, thyroid reserve, and thyroid antibodies. J
Clin Endocrinol Metab. 2002; 87:3221.
15. Diez, JJ, Iglesias, P.
Spontaneous subclinical hypothyroidism in patients older than 55 years: an
analysis of natural course and risk factors for the development of overt
thyroid failure. J Clin Endocrinol Metab. 2004; 89:4890.
16. Diez JJ, Iglesias P, Burman KD.
Spontaneous normalization of thyrotropin concentrations in patients with
subclinical hypothyroidism. J Clin Endocrinol Metab.2005;90:4124.
17. Knudsen N, Laurberg P, Rasmussen
LB, et al. Small differences in thyroid function may be important for body
mass index and the occurrence of obesity in the population. J Clin
Endocrinol Metab. 2005;90:4019.
18. Meier C, Christ-Crain M,
Guglielmetti M, et al. Prolactin dysregulation in women with subclinical
hypothyroidism: effect of levothyroxine replacement therapy. Thyroid.
2003;13:979.
19. Centanni M, Cesareo R, Verallo O,
et al. Reversible increase of intraocular pressure in subclinical hypothyroid
patients. Eur J Endocrinol. 1997;136:595.
20. Geul KW, van Sluisveld IL,
Grobbee DE, et al. The importance of thyroid microsomal antibodies in the
development of elevated serum TSH in middle-aged women: associations with
serum lipids. Clin Endocrinol. (Oxf) 1993;39:275.
21. Althaus BU, Staub JJ, Ryff-de
LËche A, et al. LDL/HDL-changes in subclinical hypothyroidism: Possible risk
factors for coronary artery disease. Clin Endocrinol.1988;28:157.
22. Parle JV, Franklyn JA, Cross, KW,
et al. Circulating lipids and minor abnormalities of thyroid function. Clin
Endocrinol. 1992;37:411.
23. Bogner U, Arntz H-R, Peters H,
Schleusener H. Subclinical hypothyroidism and hyperlipoproteinaemia:
indiscriminate L-thyroxine treatment not justified. Acta Endocrinol.
1993;128:202.
24. Caron PH, Calazel C, Parra HJ, et
al. Decreased HDL cholesterol in subclinical hypothyroidism: the effect of
L-thyroxine therapy. Clin Endocrinol. 1990;33:519.
25. Staub J-J, Althaus BU, Engler H,
et al. Spectrum of subclinical and overt hypothyroidism: effect on
thyrotropin, prolactin, and thyroid reserve, and metabolic impact on
peripheral target tissues. Am J Med. 1992;92:631.
26. Danese MD, Ladenson PW, Meinert
CL, Powe NR. Effect of thyroxine therapy on serum lipoproteins in patients
with mild thyroid failure: a quantitative review of the literature. J Clin
Endocrinol Metab. 2000;85:2993.
27. Luboshitzky R, Aviv A, Herer P,
et al. Risk factors for cardiovascular disease in women with subclinical
hypothyroidism. Thyroid. 2002;12:421-425.
28. Hak AE, Pols HA, Visser TJ, et
al. Subclinical hypothyroidism is an independent risk factor for
atherosclerosis and myocardial infarction in elderly women: the Rotterdam
Study. Ann Intern Med. 2000;132:270.
29. Lindeman RD, Romero LJ, Schade
DS, et al. Impact of subclinical hypothyroidism on serum total homocysteine
concentrations, the prevalence of coronary heart disease (CHD), and CHD risk
factors in the New Mexico Elder Health Survey. Thyroid. 2003;13:595.
30. Imaizumi M, Akahoshi M, Ichimaru
S, et al. Risk for ischemic heart disease and all-cause mortality in
subclinical hypothyroidism. J Clin Endocrinol. Metab 2004;89:3365.
31. Kvetny J, Heldgaard PE, Bladbjerg
EM, Gram J. Subclinical hypothyroidism is associated with a low-grade
inflammation, increased triglyceride levels and predicts cardiovascular
disease in males below 50 years. Clin Endocrinol. (Oxf) 2004;61:232.
32. Cikim AS, Oflaz H, Ozbey N, et
al. Evaluation of endothelial function in subclinical hypothyroidism and
subclinical hyperthyroidism. Thyroid 2004;14:605.
33. Taddei S, Caraccio N, Virdis A,
et al. Impaired endothelium-dependent vasodilatation in subclincial
hypothyroidism: beneficial effect of levothyroxine therapy. J Clin
Endocrinol Metab. 2003;88:3731.
34. Ozcan O, Cakir E, Yaman H, et al.
The effects of thyroxine replacement on the levels of serum asymmetric
dimethylarginine (ADMA) and other biochemical cardiovascular risk markers in
patients with subclinical hypothyroidism. Clin Endocrinol. (Oxf)
2005;63:203.
35. Nagasaki T, Inaba M, Kumeda Y, et
al. Increased pulse wave velocity in subclinical hypothyroidism. J Clin
Endocrinol Metab. 2006;91:154.
36. Faber J, Petersen L, Wiinberg N,
et al. Hemodynamic changes after levothyroxine treatment in subclinical
hypothyroidism. Thyroid. 2002;12:319.
37. Biondi B, Fazio S, Palmieri EA,
et al. Left ventricular diastolic dysfunction in patients with subclinical
hypothyroidism. J Clin Endocrinol Metab. 1999;84:2064.
38. Monzani F, Di Bello V, Caraccio
N, et al. Effect of levothyroxine on cardiac function and structure in
subclinical hypothyroidism: a double blind, placebo-controlled study. J
Clin Endocrinol Metab. 2001;86:1110.
39. Monzani F, Caraccio N, Kozakowa
M, et al. Effect of levothyroxine replacement on lipid profile and
intima-media thickness in subclinical hypothyroidism: a double-blind,
placebo-controlled study. J Clin Endocrinol Metab. 2004;89:2099.
40. Milionis HJ, Tambaki AP,
Kanioglou CN, et al. Thyroid substitution therapy induces high-density
lipoprotein-associated platelet-activating factor-acetylhydrolase in patients
with subclinical hypothyroidism: A potential antiatherogenic effect.
Thyroid. 2005; 15:455.
41. Rodondi N, Aujesky DA,
Vittinghoff E, et al. Subclinical hypothyroidism and the risk of coronary
heart disease: a meta-analysis. Am J Med. 2006;119:541-551.
42. Tappy L, Randin JP, Schwed P, et
al. Prevalence of thyroid disorders in psychogeriatric inpatients. A possible
relationship of hypothyroidism with neurotic depression but not with dementia.
J Am Geriatr Soc. 1987; 35:526.
43. Joffe RT, Levitt AJ. Major
depression and subclinical (grade 2) hypothyroidism.
Psychoneuroendocrinology. 1992;17:215.
44. Haggerty JJ, Stern RA, Mason GA,
et al. Subclinical hypothyroidism: a modifiable risk factor for depression?
Am J Psychiatry. 1993;150:508.
45. Monzani, F, Del Guerra, P,
Caraccio, N, et al. Subclinical hypothyroidism: neurobehavioral features and
beneficial effect of L-thyroxine treatment. Clin Invest. 1993; 71:367.
46. Haddow JE, Palomaki GE, Allan WC,
et al. Maternal thyroid deficiency during pregnancy and subsequent
neuropsychological development of the child. N Engl J Med. 1999;
341:549.
47. Helfand M, Crapo LM. Screening
for thyroid disease. Ann Intern Med. 1990;112:840-849.
48. Cooper DS, Halpern R, Wood LC, et
al. L-thyroxine therapy in subclinical hypothyroidism. A double-blind,
placebo-controlled trial. Ann Intern Med. 1984;101:18.
49. Nystr^m E, Caidahl K, Fager G, et
al. A double-blind cross-over 12-month study of L-thyroxine treatment of women
with ësubclinical' hypothyroidism. Clin Endocrinol. 1988;29:63.
50. Jaeschke R, Foyatt G, Gerstein H,
et al. Does treatment with L-thyroxine influence health status in middle-aged
and older adults with subclinical hypothyroidism? J Gen Intern Med.
1996; 11:744.
51. Meier C, Staub, JJ, Roth CB, et
al. TSH-controlled L-thyroxine therapy reduces cholesterol levels and clinical
symptoms in subclinical hypothyroidism: a double blind, placebo-controlled
trial (Basel Thyroid Study). J Clin Endocrinol Metab.2001;86:4860.
52. Caraccio, N, Ferrannini E,
Manzoni R. Lipoprotein profile in subclinical hypothyroidism: response to
levothyroxine replacement, a randomized placebo-controlled study. J Clin
Endocrinol Metab. 2002;87:1533.
53. Monzani F, Caraccio N, Kozakowa M, et al.
Effect of levothyroxine replacement on lipid profile and intima-media
thickness in subclinical hypothyroidism: a double-blind, placebo- controlled
study. J Clin Endocrinol Metab. 2004;89:2099.
54. Kong WM, Sheikh MH, Lumb PJ, et
al. A 6-month randomized trial of thyroxine treatment in women with mild
subclinical hypothyroidism. Am J Med. 2002;112:348.
55. Jorde R, Waterloo K, Storhaug H,
et al. Neuropsychological function and symptoms in subjects with subclinical
hypothyroidism and the effect of thyroxine treatment. J Clin Endocrinol
Metab. 2006;91:145.
56. Marqusee E, Hadeb ST, Utiger RD,
et al. Subclinical thyrotoxicosis. Endocrinol Metab North Am.
1998;27:37-49.
To comment on this article, contact editor@uspharmacist.com.






