US Pharm.
2007;32(12):HS-18-HS-26.
Temporomandibular disorders
(TMDs) are the most common type of facial pain condition, affecting
approximately 10% to 12% of the population, with about 25% of individuals
having at least one TMD episode during their lifetime.1
TMDs, which fall under the
category of musculoskeletal disorders, is a collective term used to describe a
number of related conditions affecting the temporomandibular joint (TMJ)
and/or masticatory muscles, all of which have three common symptoms: orofacial
pain, joint noises, and restricted jaw opening during jaw movements such as
speaking or chewing.2 Patients have reported symptoms ranging from
mild (i.e., not requiring treatment) to moderate or severe (i.e., requiring
treatment). In actuality, only about 5% to 6% of patients need treatment, with
women seeking treatment more often than men. Treatment of TMDs is challenging
and controversial in the medical and dental fields.3
Anatomy
The TMJ is a
synovial joint located at the junction of the mandible (lower jaw) and the
temporal bone of the skull (immediately in front of the ear on each side of
the head). A small cushioning disk of cartilage separates the bones, similar
to that in the knee joint, so that the mandible can slide easily. The TMJ
moves upon chewing, yawning, talking, and swallowing. It is easily located by
placing a finger on the triangular structure in front of the ear. The TMJ can
be felt in function by moving the finger slightly forward and pressing firmly
while opening the jaw to the maximum separation of the teeth and then shutting
it.
Classification of TMDs
Many terms have
been used to describe TMDs, including TMJ syndrome and TMJ disease; however,
the term TMD is the preferred term used by the American Academy of
Orofacial Pain (AAOP) and other professionals. Various classifications and
clinical diagnostic criteria exist to describe TMD.
The AAOP defines two
classifications of TMDs: muscle-related, or myogenic, TMD and joint related,
or arthrogenous, TMD.4 Occasionally, both types may be present
simultaneously, making a diagnosis difficult. Myogenic TMD, the more common
form, only involves functional alterations of the masticatory muscles around
the TMJ without TMJ problems. It usually occurs in persons with high stress
and is caused by nocturnal bruxism (teeth grinding) or day- or nighttime teeth
clenching. Arthrogenous TMD may be caused by disk displacement, recurrent
dislocation, degenerative joint disorders, hypermobility of the joint,
osteoarthritis, ankylosis, or neoplasia. Temporomandibular dysfunction occurs
when there is a displacement of the cartilaginous disk, causing pressure and
stretching of the associated muscles and sensory nerves. The characteristic
"clicking" or "popping" occurs when the mandible moves and the disk snaps into
place. Pain is also associated with spasm of the chewing muscles (i.e.,
masseter, temporalis, and pterygoid).
In the past, there was no
reliable and valid method of diagnosing TMD patients, which led to serious
misclassification of TMD cases. However, in 1992, clinical research experts
(with support from the National Institute of Dental and Craniofacial Research)
developed and published "Research Diagnostic Criteria for Temporomandibular
Disorders," which established specific operational examination procedures and
diagnostic criteria that are used in epidemiologic and clinical research for
defining TMD.5 These criteria describe a diagnosis along two
separate axes: the Axis I score provides a clinical diagnosis, while the Axis
II score provides an assessment of the psychological/behavioral aspects.
Etiology
There are many causes, both specific
and nonspecific, of TMJ pain and dysfunction, which continue to be
controversial. One reason for this controversy is that some factors are risk
factors, while others are causal in nature or purely coincidental to the TMD
problem.6,7 Although the etiologies are poorly understood, most
clinicians and researchers suggest a multifactorial etiology for TMD involving
physical, psychological, and social factors.
Physical Factors:
Sustained or repetitive loading of the masticatory system, which occurs
during parafunctional jaw activities--such as bruxism; teeth clenching; pencil
or pen chewing; gum chewing; lip biting; sucking on lips, fingers, and cheek;
and nail biting--can result in muscle hyperactivity and overloading of the TMJ.
8 Bruxism occurs in approximately 6% to 20% of the population and
between 67% and 87.5% of patients with TMD.9 Using caffeine,
tobacco, or cocaine may increase the risk of bruxism.
Trauma to the joint can occur
after a physical blow to the area or as a result of head or neck injury.
Prolonged opening of the mouth during a dental appointment (e.g., third molar
extractions),10 yawning, eating, or even excessive gum chewing can
cause trauma to the TMJ and related muscles.
Behavioral Factors:
Psychological factors that are seen in TMD patients include stress, anxiety,
and depression.11 A recent article suggested that with appropriate
early biopsychosocial intervention, acute TMD patients can be effectively
treated, regardless of the presence or absence of vulnerability to depression
symptomatology.12
Clinical Signs and Symptoms
In patients with
TMD, orofacial pain may be dull or sharp and occurs when the patient swallows,
talks, or chews. Often, the pain originates in the periauricular area;
however, it may radiate to other locations. If the joint is not properly
aligned or not working correctly, the smooth cartilage that allows the joint
to move easily may wear down, resulting in a popping or clicking noise when
the jaw opens and closes. Crepitus, a crackling or crushing noise, occurs in
more severe cases. The patient often has limited jaw-opening ability. There
may be tenderness to palpation of the TMJ via the external auditory meatus.
The adjacent muscles of the face and jaws are often in spasm, with pain and
tenderness felt in the temple area, cheek, mandible, and teeth. Patients with
TMD have similar symptoms to those of patients with other chronic pain
conditions, such as headache, toothache, earache, tinnitus, neck pain, and
other types of facial pain.13
Clinical Evaluation and
Diagnosis
Due to the
multifactorial nature of TMD, establishing a diagnosis of is difficult.
Although TMDs are a chief source of chronic orofacial pain, other etiologies
must be considered, including neoplasm, aneurysm, migraine, sinus problems,
tooth pathology (e.g., impacted wisdom tooth), nerve damage, and vascular
arteritis.
Clinical examination of the
patient involves evaluation of the range of mandibular movement by recording
the maximum mouth opening (from lower to upper front teeth) using a ruler or
caliper. If the measurement is less than 40 mm or if less than three fingers
fit in the mouth, then the patient has a decreased range of motion, which is
usually accompanied by pain and discomfort. Additionally, bilateral
auscultation of TMJ noises and gentle digital palpation of the joints and
masticatory muscles (i.e., temporalis anterior, masseter, pterygoideus
internus) should be performed.14 Any tenderness or pain in the
joints and/or muscles and joint noises (i.e., clicking or crepitus when the
patient opens and closes the mouth) should be recorded.
Magnetic resonance imaging
(MRI) or computed tomography (CT) scan of the TMJ and orofacial structures may
be performed to rule out other conditions, such as arthritis or a tumor.15
However, radiographs are sometimes difficult to interpret.
A dental examination should be
performed to detect any teeth malocclusion (e.g., crossbite). A complete
patient history should include a review of any oral habits (e.g., bruxism,
clenching, nail biting). Evaluation of the occlusal (top) surface of teeth
will determine if the patient has occlusal wear indicative of bruxism or
clenching.
In patients with chronic TMD,
behavioral, social, and emotional assessments should be performed.
Treatment
Many individuals
undergo various expensive and unproven treatments that may not be effective.
TMDs are often self-limiting and do not progress. However, in some patients
the TMJ undergoes continued degeneration, with a worsening of symptoms. Since
the primary focus of pain is around the ear, the individual may first visit an
ear, nose, and throat physician or otolaryngologist. Having eliminated the
possibility of headache, ear, or sinus problems, the next step is to consider
the possibility of TMJ pain and dysfunction. The dentist should be the next
health care provider that the individual seeks.
Management of TMJ dysfunction
may involve the use of medications or other nonsurgical or surgical options (
TABLE 1).
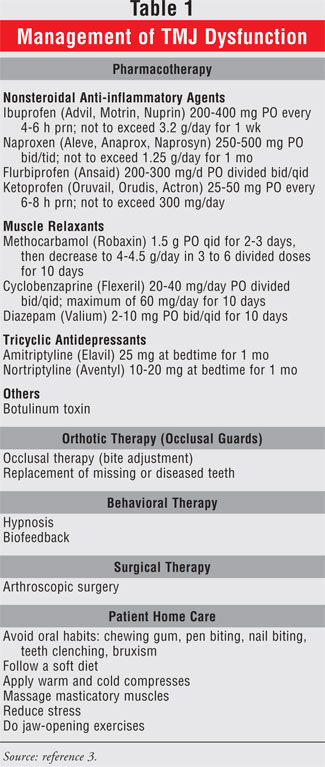
Pharmacotherapy:
In patients presenting with acute joint and muscle pain for less than three
months, treatment should be aimed at a reduction of inflammation and pain
using nonsteroidal anti-inflammatory drugs (NSAIDs)† and muscle relaxants.
3 Due to the ulcergoenic potential of NSAIDs, however, not all patients
are good candidates. Patients presenting with chronic pain, along with anxiety
or depression, may require antidepressants or anxiolytics.
Nonsteroidal anti-inflammatory
agents are the first line of treatment to reduce inflammation and pain.
Duration of therapy should be about two to four weeks. Benzodiazepines are
prescribed for significant muscle pain or spasm. Tricyclic antidepressants in
low dosages may reduce pain and nighttime bruxism. However, there have been
reports that antidepressants may trigger bruxism in nonbruxers.16
One of the newest treatment
options for TMJ-induced muscle spasms is injection of botulinum toxin.17
Botulinum toxin is a neurotoxic protein produced by the bacterium
Clostridium botulinum. When botulinum toxin A (Botox) is
injected in minute doses (15 units) into the affected muscles around the TMJ,
acetylcholine released from nerve terminals is inhibited, thus blocking
neuromuscular transmission and rendering the muscle unable to contract. It
takes about 24 to 72 hours after an injection for clinical effects to be seen.
Unfortunately, this amelioration usually lasts for only three to four months,
so most patients require repeated injections over many years. Long-term
effects of this therapy have not been studied.
Behavioral Therapy:
Reduction in stress, anxiety, and depression using behavioral modification
(e.g., relaxation therapy, hypnosis, biofeedback, meditation) and counseling
is an important part of treatment.
Occlusal Therapy:
The primary concern is to rest the muscles and joints. Individuals are
informed to eat soft foods and not to chew gum. To help reduce the incidence
of bruxism and clenching, the dentist may fabricate a soft or hard acrylic
bite plate (also referred to as an occlusal guard, night guard,
or orthopedic appliance) that is placed on the maxillary
(upper) teeth.18 This appliance is worn at night and helps prevent
the teeth from occluding, thus resting on the joint and reducing wear and
tear.
Surgical Therapy:
Arthroscopic surgery may be effective in improving the range of mandibular
movement and pain reduction, but it is mainly performed in patients with
severe joint problems.
Arthrocentesis is a surgical
procedure that washes the upper compartment of the TMJ using saline injections
into the joint space. The fluid is then withdrawn and a second injection
lavages the joint. Corticosteroids can then be injected into the joint space.
Home Care: At
home, patients should apply moist heat to the affected area at least twice a
day for no longer than 15 minutes. The various masticatory muscles involved
should be massaged several times a day until the muscle is not painful to
touch.
Other Treatments:
Ultrasonic treatment uses waves that penetrate deeper into the tissue,
increasing blood flow and reducing pain. This procedure should be done on
alternate days for about 10 minutes. Acupuncture and electronic muscle
stimulation are other methods of treatment.
Pharmacist





