US Pharm. 2006;7:10-13.
Characterized by severe elevation in
the mean pulmonary arterial pressure and pulmonary vascular resistance,
pulmonary hypertension is a devastating chronic disease with a poor long-term
prognosis. The early symptoms (e.g., difficulty in breathing, fatigue) and
later manifestations (e.g., palpitations, fainting) are shared with other
diseases. Hence, treatment may be delayed while physicians exclude other
causes for these symptoms. Results from a national registry of patients with
primary pulmonary hypertension indicated that the duration from onset of
symptoms to death averaged 2.8 years.
In recent years, new
treatments have become available for pulmonary hypertension, particularly for
pulmonary arterial hypertension. The treatments, which include anticoagulants,
calcium channel blockers, and prostacyclins, prolong survival and provide
clinical improvement, but they can be expensive. Although effective management
might be possible with early detection, most people are diagnosed with
pulmonary hypertension in later stages of the disease, making treatment more
difficult and less successful. Pulmonary hypertension is reported on hospital
records and death certificates either as primary pulmonary hypertension or as
pulmonary hypertension secondary to another underlying condition or disease.
Pulmonary hypertension might be secondary to congenital heart disease,
valvular heart disease, chronic thromboembolic disease, lung diseases, liver
diseases, sleep-disordered breathing, hypoxemia, lupus, scleroderma,
rheumatoid arthritis, vasculitis, or HIV infection. Limited national
statistics are available regarding pulmonary hypertensive diseases. Although a
rare condition, primary pulmonary hypertension as the reported cause of death
has increased since 1979, and the number of all cases is likely to be higher
than reported numbers because of difficulties in diagnosis.
Hospitalizations
During 1980 to
2002, the estimated number of hospitalized patients with pulmonary
hypertension as the diagnosis tripled for the total U.S. population. Compared
with estimated numbers of hospitalizations in 1980, the numbers in 2002 were
two times higher among men and three times higher among women. Rates of
hospitalization for pulmonary hypertension among women were higher than those
in men, but only after 1995. In 2002, the hospitalization rate (per 100,000
population) for pulmonary hypertension as the diagnosis was 95.3 for women and
82.3 for men. The number of hospitalizations and hospitalization rates
increased among all age-groups in the U.S. population. The greatest increase
in hospitalization rates was among adults 75 years and older.
During 1980 to 2002, the
greatest increase in hospitalizations for pulmonary hypertension occurred in
men 85 years and older and in women 65 years and older. Because of major
increases in hospitalizations among women 85 years and older during 2000 to
2002, women had higher hospitalization rates than men did in this older
age-group.
During 1980 to 2002, trends in
the most commonly reported principal diagnoses changed. From 1980 to 1984, the
most commonly reported principal diagnoses among hospitalized patients with a
diagnosis of pulmonary hypertension were chronic lower respiratory diseases
(42%), followed by pulmonary hypertension (12.8%) and cardiovascular diseases
(6.8%). By 2000 to 2002, heart failure (18.7%) was the most commonly reported
principal diagnosis among hospitalized patients with a diagnosis of pulmonary
hypertension; this was followed by chronic lower respiratory diseases (12.9%).
During 2000 to 2002, pulmonary hypertension was the principal diagnosis in
only 4.2% of hospitalizations involving a diagnosis of pulmonary hypertension.
Declines in reporting pulmonary hypertension and chronic lower respiratory
disease and the increase in reporting heart failure as the principal diagnosis
in these cases were observed among all groups defined by sex and age.
Among those younger than 45
years who were hospitalized, the principal diagnosis was more likely to be
pulmonary hypertension (26%) and congenital malformations (22.9%) during 1980
to 1984; however, by 2000 to 2002, these conditions had declined as the
principal diagnoses among hospitalized patients with pulmonary hypertension as
the listed diagnosis. Other cardiovascular diseases (29.8%), other respiratory
diseases (9.8%), pulmonary hypertension (9.5%), and chronic lower respiratory
diseases (7.1%) were the major principal diagnoses from 2000 to 2002. Among
patients younger than 45 years who were hospitalized for pulmonary
hypertension, influenza and pneumonia (4.6%), congenital malformations (4.3%),
complications related to specific procedures (3.9%), cellulitis and abscesses
(3.6%), and complications related to pregnancy and childbirth (3.2%) were
principal diagnoses.
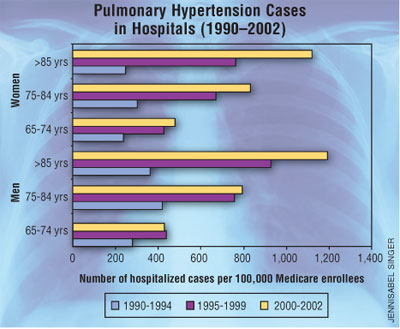
Medicare Claims
During 1990 to
2002, the annual number of hospitalizations among Medicare enrollees 65 years
and older who had pulmonary hypertension as a diagnosis tripled from 55,516 to
187,205. Until 1999, men were more likely than women to be hospitalized for
pulmonary hypertension. Increases in numbers of Medicare hospitalizations for
pulmonary hypertension were observed among all groups defined by race and age.
Hospitalization rates were higher for blacks than for whites. Hospitalization
rates increased for all age-groups, but the rates were not the highest among
adults ages 85 years and older until after 1995. By 2000 to 2002,
hospitalization rates were higher among women ages 65 to 74 years and 75 to 84
years, and whites ages 85 years and older had higher hospitalization rates
than did blacks in the same age-group.
Conclusion
The high proportion
of pulmonary hypertension-related deaths and hospitalizations that occurred
among adults 65 years and older suggests that as the proportion of older
adults in the U.S. population increases, pulmonary hypertension might continue
to be a more frequent diagnosis, particularly with concomitant chronic heart
failure. Because the majority of patients with pulmonary hypertension are
older adults, the burden of chronic disability and morbidity on the Medicare
system and families will increase.
Prevention efforts, including
broad-based public health efforts to increase awareness of pulmonary
hypertension and foster appropriate diagnostic evaluation and timely
treatment, should be considered. Although multiple predisposing factors and
associated conditions have been identified for pulmonary hypertension, the CDC
believes that the causal roles and strengths of association have not been well
established. Thus, it is not possible to establish preventive measures
regarding risk factor reduction.
To comment on this article, contact
editor@uspharmacist.com.






