US
Pharm. 2006;5:HS-21-HS-33.
The impact of licit (i.e.,
alcohol and nicotine used legally), illicit, and nonmedical prescription drug
abuse and dependence in the United States is a well-documented matter
affecting many individuals in the general population. A substantial number of
patients served daily by pharmacists in community, hospital, and other health
care facilities are therefore abusing or are dependent on alcohol, other
drugs, or a combination (AOD). Despite this, a recent report concerning
substantial abuse of prescription medication in the U.S. reported that many
pharmacists are poorly trained to deal with alcohol or drug abuse.1
As one of America's most
trusted professionals, the public expects pharmacists to respect the proper
use of the medicines that they dispense to their patients.2 Just as
in their patients, though, alcohol and other drug abuse and dependence are
affecting the lives of a number of pharmacists, leading some researchers to
call pharmacists our society's "drugged experts."3 In
reality, while pharmacy students and pharmacists report somewhat higher
lifetime and past-year prevalence of prescription drug use of opioids and
anxiolytics than comparable groups of college students or the general
population, respectively, lifetime and past-year prevalence of illicit drug
use overall is less likely to be reported by pharmacy students and pharmacists.
4,5
Although not a widely
discussed or well-researched topic, the issue of pharmacists impaired by
prescription, illegal, and legal drug abuse needs to be addressed. Beginning
in pharmacy college, some students may develop an air of invulnerability and
immunity to addiction, perhaps because of an advanced understanding of drug
action. What begins as recreational college AOD use may, for some individuals,
develop into a complicated pattern of AOD abuse or dependence intended to
produce a "sense of well-being" without an overt manifestation of intoxication
or side effects.6,7 This concept of balancing drug effects, also
called titration, refers to a practice in which pharmacists use their
pharmacological knowledge to balance drug actions and reactions by "enhancing,
neutralizing, or counteracting specific drug effects through ingesting
multiple types of drugs."8
When a pharmacist
experiences drug impairment, the responsibility to protect the public
ultimately falls upon the pharmacy profession, as represented by the licensing
boards and professional societies. The pharmacy practice act of each state
describes the parameters of professional activity. When a pharmacist violates
these laws, he or she is subject to punitive board action, such as license
suspension or revocation. In addition to board prosecution, state pharmacy
professional organizations can organize, sponsor, or support a pharmacist
recovery network (PRN) program. These programs offer confidential support and
assistance to pharmacists who are impaired by drug or alcohol abuse or
dependence, and/or emotional or mental health problems.9
Whether through board action
or collegial PRN intervention, the impaired pharmacist is taken out of
practice until the impairment is resolved. Furthermore, since AOD abuse and
dependence exists in nondistinct shades of gray, pharmacists (and other health
care professionals) are often ill-prepared to deal effectively with AOD abuse
and dependence by patients, others in the profession, or themselves.10
Scope of the Problem
The National
Survey on Drug Use and Health in 2004 reported that 22.5 million Americans
ages 12 years and older abused or were dependent on AOD during the year before
the survey.11 This rate of abuse or dependence equals 9.4% of the
U.S. population. Additionally, more than six million individuals reported
using nonprescribed psychotherapeutic agents.
While pharmacists may be at
greater risk of using prescription drugs than the general population, there is
currently no evidence that total lifetime or past-year drug use by pharmacists
significantly exceeds that of other major groups of health care professionals
or the general population. 12 However, it appears that the greatest
threats to pharmacists are nonmedical opiate, stimulant, and antianxiety drug
use (due to easy availability), as well as legal drugs, alcohol, and nicotine.
12 Most nonprescribed opioid and antianxiety drug use by pharmacists is
taken for self-diagnosed ailments, while most stimulant use is taken to
facilitate performance.13 Consistent with previous research, a
study found that the majority of pharmacists who used these drugs initially
did so after leaving college.14 In addition, 40% of pharmacists
reported that they had used a prescription drug without a physician's
authorization, and 20% reported that they had done so five or more times in
their lifetime.14
What Are Chemical Abuse,
Dependence, and Addiction?
The terms abuse
, dependence, and addiction appear to be confusing to the
public and health care professionals since there is both a colloquial (which
is how we will be using these terms) and a diagnostic use of the terms for
alcohol or any other substance overuse. The term substance abuse is
commonly used as a substitute for any use of an illegal substance. However,
since there is no substance that is not a chemical or drug, the term
substance is problematic. In contrast, treatment professionals limit the
use of the term substance abuse to describe the symptoms of individuals
who meet the specific criteria for a medical diagnosis of abuse as listed in
the Diagnostic and Statistical Manual of Mental Disorders, as discussed
below. 15 Substance (i.e., drug, chemical) abuse is a pattern of
AOD overuse that produces many adverse results during continual use of the
chemical. The diagnostic characteristics of chemical abuse include at least
one of the following behaviors determined to be present in a 12-month period
by a qualified assessment professional:
•Failure to carry out
obligations at home or work.
•Recurrent social or
interpersonal problems.
•Continual use of the
drug in circumstances that present a hazard (e.g., driving a car), and legal
problems, such as arrests.
•Use of the drug is
persistent, despite personal problems caused by the effects of the chemical on
oneself or others.
The term AOD dependence
, on the other hand, has been medically defined as a group of behavioral
and physiological symptoms that indicate the continual, compulsive use of
chemicals in self-administered doses, despite the problems related to the use
of the drug.15 The diagnostic characteristics of dependence,
popularly called addiction, include the presence of at least three of
the following behaviors in a 12-month period, as determined by a qualified
assessment professional:
•Tolerance.
•Signs of withdrawal
(vary by drug class).
•Use of larger
amounts of the drug or for a longer period of time than intended.
•Persistent desire or
unsuccessful efforts to cut down or control use.
•Continual use
despite adverse consequences.
•An excessive amount
of time and effort spent obtaining the drug.
•Social,
occupational, or recreational activities given up or time spent doing them
reduced.
Tolerance is evident when
the same amount of drug results in a diminished effect or increased amounts of
the drug are needed to achieve the desired result or level of intoxication.
Withdrawal signs and symptoms signify physiological and psychological changes
that occur when the body's concentration of the chemical declines in a person
who has been a heavy user. Given the neurophysiological changes occurring with
chronic AOD abuse, withdrawal symptoms are typically actions opposite to those
of the drug. For example, alcohol's sedative effect results in increased
autonomic hyperactivity when alcohol is withdrawn. When signs of tolerance or
withdrawal are seen, the AOD abuser is said to be "physiologically dependent."
Pharmacy's Role in Drug
Abuse Prevention and Education
Generally,
pharmacists receive inadequate education on drug abuse.16 More
specifically, pharmacy students and pharmacists are insufficiently trained to
identify, intervene, or treat patients and coworkers with drug abuse problems.
17,18 In a study published by the Center on Addiction and Substance
Abuse (CASA) in 2005, only 48% of the 1,030 registered pharmacists surveyed
had received any training in preventing drug diversion.1 Moreover,
only 49% had received training in identifying abuse or dependence since
graduation from pharmacy college. The perception by practicing pharmacists is
that proficiency in drug abuse prevention, education, and even treatment
options must be addressed in pharmacy college.16 The CASA study
also revealed that only about half of the pharmacists surveyed rated the
substance abuse education and training they received in college as good or
excellent.
In addition to drug abuse
education and training before and after graduation from pharmacy college,
opportunities for specialization in residency programs should be provided, and
pharmacist involvement in community service and drug abuse treatment research
should be encouraged.19 In 2003, the American Society of
Health-System Pharmacists published a position statement, noting that
pharmacists have a distinct opportunity to have a fundamental role in drug
abuse prevention, education, and assistance.20 Given the extent and
consequences of potential chemical abuse in the workplace, pharmacy must
accept a responsibility for educating its own profession. As health care
professionals with an abundance of drug knowledge and responsibility,
pharmacists should shoulder the responsibility of leading drug abuse
prevention and education efforts. Pharmacists are also needed to assist in
patient care, employee health, and community activities. The most important
activity the profession can facilitate is promoting the understanding of drug
abuse and dependence among pharmacy students and pharmacists.
Educating Pharmacists and
Pharmacy Students About Drug Abuse and Dependence
Pharmacy colleges
in several states have begun to more proactively educate the profession in
this long-neglected area. While guidelines have been published for including
this topic in pharmacy education, the suggestions have been mostly ignored.
21 Several exceptions are the 20 hours of core content on drug abuse and
dependence offered at the University of Maryland School of Pharmacy and the
eight hours of core content in the main pharmacotherapy course at the
University of Texas College of Pharmacy, which also offers a five-hour
orientation program on the disease of chemical dependence, intervention, and
resources for students entering the college. In addition, the University of
Nebraska College of Pharmacy includes six hours of core content in its
pharmacotherapy course and offers a substance abuse elective that
approximately 80% of its students complete. The university provides a brochure
to all students and faculty annually that details its chemical dependency
assistance program and local resources, and it provides a program overview
during new student orientation.
In 2000, the Texas State
Board of Pharmacy approved four policies for implementation: (1) to support
the concept of more training in chemical dependency for Texas pharmacists; (2)
to support the attitude that such training is needed to protect the public;
(3) to encourage Texas colleges of pharmacy to offer required lectures on
chemical dependency; and (4) to move toward setting minimum standards for
certification of pharmacists trained in chemical dependency. While the final
policy has not yet been implemented, the University of Texas School of
Pharmacy has produced 12 hours of chemical dependency training ("Because They
Trust Us" continuing education videotapes) and a micro-Web C.E. learning
series, "Neurobiology of Addiction."22
The Basics: What
Pharmacists Need to Know About AOD Abuse and Dependence
All health care
professionals are being called to action in the effort to address the problems
of drug abuse and dependence in the U.S.23 At a minimum,
pharmacists should be able to screen for these problems, assess their
severity, refer individuals to appropriate levels of care, and provide
appropriate counseling for those in recovery. To perform these activities,
pharmacists should be educated about them and possess an ethic that promotes
the necessary deployment of skills. For instance, pharmacists need logistical
support in their practice environment to provide these services. This entails
sufficient time to engage patients in counseling and an area that affords
privacy and confidentiality. Pharmacy owners and managers, as well as
dispensing pharmacists, need to make workplace accommodations that demonstrate
the commitment to this professional activity.
Screening patients for
substance abuse disorders is essential. Consider the number of prescriptions
dispensed with an auxiliary label that warns patients against the use of
alcohol "while taking this medication." For individuals who are dependent on
alcohol, such advice would be difficult to follow. The pharmacist who advises,
"If you find that you are unable to refrain from alcohol use during the period
of prescription therapy, I strongly recommend that you seek assistance," may
spark a turning point in the life of an individual who otherwise feels in
total control of alcohol.
Pharmacists also practice in
varied settings. For those in clinics, it may be practical to follow up a
positive drug screening with assessment questions that estimate the dose,
frequency, and duration of AOD overuse. A patient's responses to these
questions will reveal information that will affect the treatment of other
conditions (e.g., diabetes, hypertension, anticoagulation therapy) and perhaps
suggest the need for treatment of an AOD abuse or dependence disorder.
Clinical pharmacists can easily become frustrated when the dependent patient
displays nonadherence to medication regimens and disease management advice.
Until the chemical dependence is diagnosed and treated, the adverse effects of
a patient's substance abuse on medication adherence and treatment outcomes for
other illnesses are likely to continue.
In community pharmacy
practice, assessment is less practical. Unless the pharmacist has made a
concerted effort to spend time with patients in confidential counseling, the
exigencies of dispensing leave little time for assessment. The advent of
medication therapy management may provide sufficient incentive for community
pharmacists to make the necessary arrangements to routinely engage in more
therapeutic conversations with patients regarding their pharmacotherapy.
24
Pharmacy practice
necessitates educating students and pharmacists on the identification of
abusing and dependent patients, referral to evaluation and support resources
for individuals affected by AOD use or those concerned about them, common
prescription scams such as patient claims of "lost" or "stolen" narcotic
analgesics and prescription forgeries, and serving as a resource for
assistance-related materials and other information (patient resources).
Updating the paradigm of pharmacy as the gatekeeper to include pharmacy as the
educator includes enhancing the role of the pharmacist in supporting addiction
recovery. For example, pharmacists can counsel on the use of addicting and
mood-altering medications, provide appropriate counseling about what is not
addiction, and counter "addiction phobias" for those patients (e.g., hospice
patients) who require significant pain control but fear becoming addicted to
the prescribed medication.
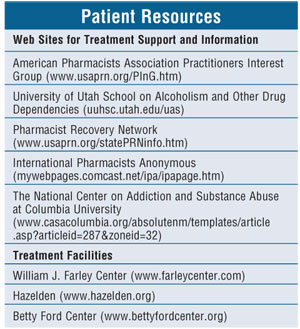
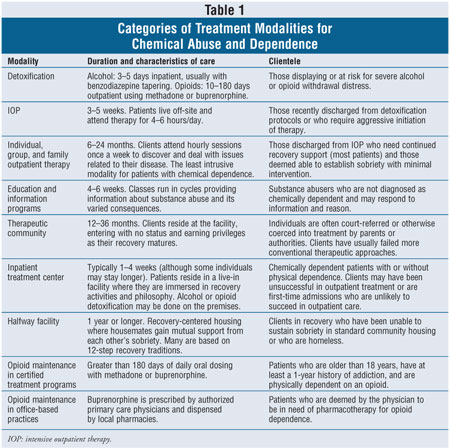
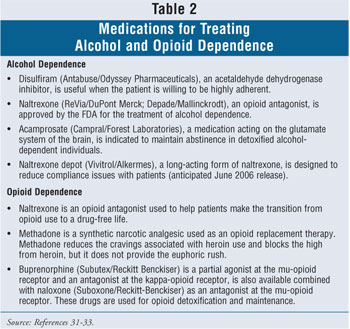
A multitude of resources exists to treat AOD abuse and dependence disorders. The major treatment options available in the community are listed in table 1, and the currently available medications for alcohol and opiate dependence treatment are listed in table 2. The thorough assessment is a critical prerequisite to a proper referral. Little is gained when needs and services are mismatched. Much time and money are wasted by individuals who minimize the severity of their AOD abuse or dependence and participate in an inadequate level of care.
Taking Care of Our Own:
Pharmacy Profession Response to Chemical Abuse and Dependence in Pharmacists
The goals of
ethical standards and licensing laws in the health professions include
protecting the public and establishing the boundaries of professional conduct.
Stepping outside the standards of conduct and violating practice regulations
expose errant practitioners to sanction. However, nonpunitive options increase
the likelihood that pharmacists will refer themselves for intervention and
that other pharmacists will refer an impaired colleague. Employee assistance
programs (EAPs) utilize a rehabilitative approach to chemical abuse and
dependence in the workplace. For over 50 years, these programs have offered
assistance to workers with various problems, such as AOD overuse, that
negatively affect their job performance.25 This approach offers
confidential assistance to employees who request help. Workers who enter an
EAP are afforded an opportunity to deal with a substance use disorder in a
therapeutic setting while the worker's supervisor relies solely on job
performance criteria for making decisions about continued employment.
The PRN providers use the
rehabilitative approach to assist pharmacists who abuse or are dependent on a
drug. PRN programs limit their outreach and intervention services to
pharmacists, pharmacy students, and pharmacy technicians. Umbrella programs
offer assistance to multiple professions for various problems, including
psychoactive substance dependence assistance, through a central provider. Both
programs are modeled after EAPs and identify individuals for rehabilitative
intervention, rather than punitive action.
PRN services, available in
all 50 states, offer an alternative to board of pharmacy license sanctions
when dealing with a pharmacist who has AOD problems.26 Pharmacists
who need and want confidential help can contact their state PRN. Organized in
1982 by the American Pharmacists Association (APhA, formerly the American
Pharmaceutical Association), the program is dedicated to the early
identification, intervention, and treatment of drug-affected pharmacists,
pharmacy students, and technicians. Pharmacists who have an AOD problem can
call their state PRN to ask for confidential advice and assistance.
Information is collected and the individual is referred for follow-up to a
counselor or a chemical dependency assessment and treatment specialist. Early
discovery of such individuals preserves both professional health and public
safety.
Identifying Drug Problems
in Coworkers
Most corporate
chain store retailers and hospital pharmacies use statistical analysis to
determine worker access to specific drugs on a periodic basis (e.g., monthly).
If a particular employee appears to consistently access controlled drugs more
often than his or her peers without sufficient cause, a more formal
investigation is begun, perhaps instituting the use of video cameras or
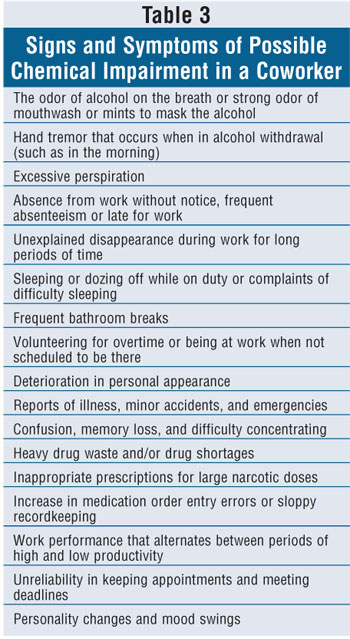
auditing the site. Behaviorally, however, there are several signs and symptoms
of AOD abuse that coworkers may notice (table 3). In fact, some of these
markers may indicate the type of impairment. For example, unexplained work
absences may indicate an alcohol abuse or dependence problem, since home is
the more convenient place to store and access alcohol. In contrast,
consistently volunteering to work overtime or work with controlled substance
inventory, and arriving at work at unscheduled times, provides an impaired
coworker the opportunity to access controlled substances that are not
available at home. Unfortunately, such symptoms are more easily identified in
hindsight than before a coworker is identified to have an AOD disorder.
Probably one of the most difficult
professional decisions a pharmacist can make is to confront a coworker with an
AOD problem. Given the seriousness of dependence disease and its treatment,
intervention can be awkward. More importantly, pharmacists should consider
that in retrospect, many colleagues feel that an intervention probably saved
their life.8 Also, while these individuals may have been devastated
at the time of their discovery, the reality is that the majority do
successfully return to work, which will be detailed shortly. Furthermore,
given the shortage of pharmacists, it is probable that many of these
individuals will be allowed to resume their profession if they cooperate with
treatment, which may include compensation to the employer for the diverted
drugs in cases of criminal diversion.20
Recovery Assistance
Programs, Risk Factors for Relapse, and Treatment Success
Once an
individual's AOD problem surfaces, treatment decisions are generally tailored
to his or her needs (tables 1, 2). While discussing the diverse treatment
options available in a meaningful way is beyond the scope of this article,
certain basic goals of treatment include matching the patient to the correct
level of care, such as deciding whether an individual is better suited for
inpatient versus outpatient treatment.27 Beyond placement, the
fundamental facets of treatment include individual and group therapy,
pharmacotherapy when appropriate, urine drug screens, and 12-step
facilitation. Twelve-step programs include Alcoholics Anonymous, Narcotics
Anonymous, Caduceus (for health care professionals), International Pharmacists
Anonymous (a psychosocial support group specifically for pharmacists), and
International Doctors in Alcoholics Anonymous (a support group that now
includes pharmacists in its membership, regardless of pharmacy degree).
There is inadequate research
assessing risk factors for relapse or treatment success of recovering
pharmacists. In a retrospective cohort study of 292 health care professionals,
including pharmacists enrolled in Washington state's Physicians Health
Program, only about 25% of the study population had one or more relapses.
28 The risk of relapse was significantly higher in health care
professionals who used a major opioid, had a coexisting psychiatric illness,
or reported a family history of an AOD disorder. Coexisting risk factors and
previous relapse also increased the likelihood of relapse.
In 1988, a survey examined
pharmacist assistance programs in all 50 states and the District of Columbia.
29 The survey reported that only 20% of impaired pharmacists in these
treatment programs voluntarily disclosed their chemical use problem. Most
importantly, just over 88% successfully completed treatment and returned to
practice. These studies suggest that the goal of returning a recovering
pharmacist to practice with the proper aftercare and monitoring program is
realistic and almost always successful.
Since 1982, APhA has worked
to adopt and institute a policy of treatment, prevention, and rehabilitation
of pharmacists who use AOD. For over 20 years, APhA has actively supported the
pharmacy section of the Utah School on Alcoholism and Other Drug Dependencies
in Salt Lake City. The purpose of this annual weeklong program is to bring
together pharmacists and pharmacy students with various state PRN
coordinators, state administrators, industry representatives, and interested
individuals from around the country to listen to updates on various aspects of
AOD intervention and treatment.
The Health Professional
Students for Substance Abuse Training (HPSSAT) is a project of the Physician
Leadership on National Drug Policy that is free to join.30 The goal
of this organization is to have all graduating health professional students
develop the skills to screen, diagnose, and provide appropriate intervention
for patients with an AOD problem. Through HPSSAT, students can be advocates
for local and national educational reform of substance abuse education and
treatment training.
Conclusion
Agencies such as the
Drug Enforcement Administration, state departments of health, boards of
pharmacy, state pharmacy associations, and colleges of pharmacy should
coordinate discussions about AOD use among patients, as well as pharmacists
and pharmacy students. Dissemination of information (e.g., continuing
education opportunities) relating to the warning signs of drug abuse and
sources of help for those affected by AOD should be continual goals of these
agencies. Colleges of pharmacy should pay particular attention to providing
instruction on the neurobiological and psychological processes of AOD
dependence and, in particular, the threats posed by alcohol, nicotine,
opioids, stimulants, and antianxiety drugs, since these are the drugs most
associated with abuse, dependence, and health problems. Efforts to dissuade
pharmacists and pharmacy students from using AOD may not immediately produce
visible results. Ultimately, however, academic and governmental agencies need
to make every reasonable effort to educate both future and practicing
pharmacists about these issues.
While the rates of AOD abuse
or dependence among pharmacists are no greater than in the general population,
the consequences of any impairment can have adverse effects on patients.
People entrust their personal welfare and safety to those in the health
professions. The profession, in turn, has an ethical obligation to ensure that
its practitioners can discharge their duties with skill and safety. Policies
should promote early discovery of professionals who overuse AOD in order to
minimize the period of time that patients are at risk of being harmed.
Dedicated to the memory of
Lance Smith, BS, pharmacy class of 2001, University of Rhode Island, Kingston.
REFERENCES
1. The National
Center on Addiction and Substance Abuse at Columbia University. Under the
Counter: The Diversion and Abuse of Controlled Prescription Drugs in the U.S.
New York, NY; 2005.
2. Gallup
Organization. Honesty/Ethics in Professions. Available at:
www.gallup.com/poll/content/login.aspx?ci=14290. Accessed August 26, 2005.
3. Dabney D,
Hollinger R. Illicit prescription drug use among pharmacists: evidence of a
paradox of familiarity. Work Occupations. 1999;26:102.
4. Office of Applied
Studies. Results from the 2002 National Survey on Drug Use and Health: Summary
of national findings. Rockville, Md.; Substance Abuse and Mental Health
Services Administration; 2003. NHDUH series H-22; U.S. Department of Health
and Human Services publication SMA 03-3836.
5. Kenna GA, Wood MD.
Substance use by pharmacy and nursing practitioners and students in a
northeastern state. Am J Health Syst Pharm. 2004;61:921-930.
6. McAuliffe WE,
Santangelo SL, Gingras J, et al. Use and abuse of controlled substances by
pharmacists and pharmacy students. Am J Hosp Pharm . 1987;44:311-317.
7. McGuffey EC.
Lessons from pharmacists in recovery from drug addiction. J Am Pharm Assoc
. 1998;38:17.
8. Dabney D. A
sociological examination of illicit prescription drug use among pharmacists
[unpublished dissertation]. Gainesville, Fla: University of Florida; 1997:97.
9. Tommasello AC.
Substance abuse and pharmacy practice: what the community pharmacist needs to
know about drug abuse and dependence. Harm Reduct J. 2004;1:3. Available at:
www.harmreductionjournal.com/content/pdf/1477-7517-1-3.pdf. Accessed August
25, 2005.
10. Lawson KA, Wilcox
RE, Littlefield JH, et al. Educating treatment professionals about addiction
science research: demographics of knowledge and belief changes. Subst Use
Misuse. 2004;39:1235-1258.
11. Office of Applied
Studies. Results from the 2004 National Survey on Drug Use and Health: Summary
of national findings. Rockville, Md.; Substance Abuse and Mental Health
Services Administration; 2005. NHSDA series H-282; U.S. Department of Health
and Human Services publication SMA 03-3836.
12. Kenna GA, Wood
MD. Prevalence of substance use by pharmacists and other health professionals.
J Am Pharm Assoc. 2004;44:684-693.
13. McAuliffe WE,
Rohman M, Santangelo S, et al. Psychoactive drug use among practicing
physicians and medical students. N Engl J Med. 1986;315:805-810.
14. Dabney D. Onset
of illegal use of mind-altering or potentially addictive prescription drugs
among pharmacists. J Am Pharm Assoc. 2001;41:392-400.
15. Diagnostic and
Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision).
Washington, D.C.: American Psychiatric Association; 2000.
16. Graham A, Pfeifer
J, Trumble J, Nelson ED. A pilot project: continuing education for pharmacists
on substance abuse prevention. Subst Abus . 1999;20:33-43.
17. Baldwin JN, Light
K, Stock C, et al. Curricular guidelines for pharmacy education: substance
abuse and addictive disease. Am J Pharm Educ. 1991;55:311-316.
18. Dole EJ,
Tommasello A. Recommendations for implementing effective substance abuse
education in pharmacy practice. In: Haack MR, Adger H, eds. Strategic Plan
for Interdisciplinary Faculty Development: Arming the Nation's Health
Professional Workforce for a New Approach to Substance Use Disorders.
Providence, R.I.: Association for Medical Education and Research in Substance
Abuse (AMERSA); 2002:263-271.
19. Cobaugh DJ.
Pharmacist's role in preventing and treating substance abuse. Am J Health
Syst Pharm. 2003;60:1947.
20. ASHP statement on
the pharmacist's role in substance abuse prevention, education and assistance.
Am J Health Syst Pharm. 2003;60:1995-1998.
21. Baldwin JN, Dole
EJ, Levine PJ, et al. Survey of pharmacy substance abuse course content. Am
J Pharmaceut Educ. 1994;58(suppl):47S-52S.
22. University of
Texas College of Pharmacy. "Because They Trust Us" continuing education
videotapes and micro-web C.E. learning series on the "Neurobiology of
Addiction." Available at: www.utexas.edu/pharmacy/ce/BTTU.html. Accessed
February 9, 2006.
23. Haack MR, Adger
H. Strategic plan for interdisciplinary faculty development: arming the
nation's health professional workforce for a new approach to substance use
disorders. Substance Abuse. 2002;23:1-21.
24. American
Pharmacists Association. Understanding Medicare Reform: What Pharmacists
Need to Know (monograph 2): Medication Therapy Management Services and Chronic
Care Improvement Programs. Washington, DC: APhA; 2004.
25. Steele PD, Trice
HM. A history of job-based alcoholism programs: 1972-1980. J Drug Issues
. 1995;25:397-422.
26. Pharmacist
Recovery Network. Available at: www.usaprn.org. Accessed January 15, 2006.
27. Nace EP.
Achievement and Addiction: A Guide to the Treatment of Professionals. New
York, NY: Brunner/Mazel; 1995.
28. Domino KB,
Hornbein TF, Polissar NL, et al. Risk factors for relapse in health care
professionals with substance use disorders. JAMA. 2005;293:1453-1460.
29. McNees GE, Godwin
HN. Programs for pharmacists impaired by substance abuse: a report. Am Pharm
. 1990;NS30:33-37.
30. Health
Professional Students for Substance Abuse Training. Available at:
www.hpssat.org/about/index.html. Accessed February 9, 2006.
31. Kenna GA, McGeary
JE, Swift RM. Pharmacotherapy, pharmacogenomics and the future of alcohol
dependence therapy. Am J Health Syst Pharm. 2004;61(21)part
1:2272-2279.
32. Kenna GA, McGeary
JE, Swift RM. Pharmacotherapy, pharmacogenomics and the future of alcohol
dependence therapy. Am J Health Syst Pharm . 2004;61(22)part
2:2380-2390.
33. Gerada C. Drug
misuse: a review of treatments. Clin Med. 2005;5:69-7 3.
To comment on this article, contact editor@uspharmacist.com .






