US Pharm, 2008;33(11):20-22.
Agitation and psychosis are common in adults with dementia and are associated with serious clinical consequences (e.g., more rapid cognitive decline).1 While the atypical antipsychotic agents have been widely used in seniors with dementia--albeit based essentially on data from younger study populations--they have been proven to cause metabolic adverse effects, including weight gain, type 2 diabetes mellitus, and dyslipidemia.1,2
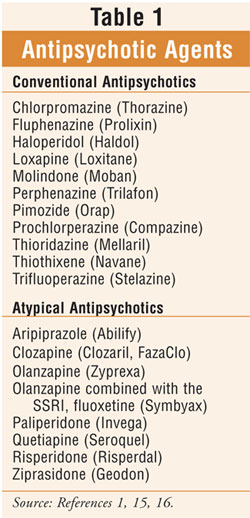
The increased risk of death associated with atypical antipsychotic agents in elderly patients with dementia-related psychosis also applies to the conventionalantipsychotic agents (TABLE 1). This is the conclusion summed up in an FDA alert on June 16, 2008, notifying health care professionals about the current analysis of data concerning these drugs.3 Manufacturers of conventional antipsychotic agents are being required by the FDA to add a Boxed Warning and Warning to the drugs' prescribing information regarding the risk of mortality in elderly patients treated for dementia-related psychosis; this information is similar to the Boxed Warning and Warning added to the prescribing information of the atypical antipsychotic agents in 2005.3 This requirement falls under the FDA's new authority to require safety label changes provided in Title IX of the FDA Amendments Act of 2007.3
The results of two observational epidemiological studies in Canada were recently published discussing the risk of death in patients treated with conventional antipsychotics.4,5 One study found atypical antipsychotics were associated with increased mortality as compared to no antipsychotic use; conventional antipsychotic use demonstrated a marginally higher risk of death compared with atypical antipsychotic use. This particular study did not report the causes of death.4 Another study found the risk of death in the patient group receiving conventional antipsychotics comparable to, or possibly greater than, the risk of death in the patient group receiving atypical antipsychotics.5 In this study, the causes of death with the highest relative risk were cardiac disease and cancer.5
The mechanism for increased death associated with these antipsychotics is not completely understood, and there were limitations in the methodology of each study.3,6 Given these data and other existing evidence, however, the FDA has determined that the overall weight of evidence shows that conventional antipsychotics share the increased risk of death in geriatric patients with dementia-related psychosis that has been seen with the atypical antipsychotics.3,6 Furthermore, it is important for pharmacists and other health care professionals to be aware of the fact that antipsychotic agents, whether conventional or atypical, are not indicated for the treatment of dementia-related psychosis.3 That does not mean that they cannot be utilized in individuals with this condition; however, it does mean that extreme caution should be taken when these agents are prescribed for vulnerable individuals.6 Evaluating the risks versus benefits of antipsychotic drug therapy should always be considered as part of the decision-making process. A summary of updated issues regarding antipsychotic medication use in seniors appears in TABLE 2.

Prevalence of Dementia
and Related Agitation and
Psychosis
Dementia is defined as global cognitive impairment that occurs in a clear sensorium (versus stupor suggesting delirium) and is irreversible; it is not a disease, but rather a syndrome.7 Alzheimer's disease is the most common type of dementia.1 While the prevalence of dementia ranges from 5% to 15% in U.S. adults over the age of 65, its effect will be increasingly important globally as the estimated number of patients with dementia is expected to reach 48 million worldwide by the year 2020.1,8-11 To understand the significance of this growing problem, pharmacists should note that up to 60% of community-dwelling patients with dementia develop behavioral and psychiatric symptoms as compared with greater than 80% of those residing in nursing homes.1,12,13
Preventing Misuse of
Psychotropic Drugs in Seniors
Antipsychotic agents have been referred to as probably one of the most misused categories of medications in the geriatric population.14 Data indicate that greater than 50% of nursing home residents receive at least one psychotropic medication (e.g., antidepressant, antipsychotic, sedative-hypnotic).14 According to Kane et al, preventing the misuse of antipsychotics and other psychotropic agents in the elderly may be accomplished through consideration of the following14:
Clarify Symptoms: This process will help determine if and what factors caused the symptoms to be precipitated.
A Medical Evaluation: This should be thoroughly performed since psychological symptoms in geriatric patients may be caused or exacerbated by medical conditions. This will protect from the assumption that symptoms are due to psychiatric conditions requiring the initiation of psychotropic drug therapy.
Diligence in identifying the underlying causes of dementia-related agitation and psychosis enables the clinician to aggressively treat the causes with the most appropriate pharmacological and nonpharmacological interventions.6
Accurate Psychiatric Diagnosis: This drives appropriate therapy for psychological symptoms that may present nonspecifically in elderly adults. Consultation with a psychiatrist or psychologist with specialized training in and experience with geriatric patients is especially helpful when available. Pharmacists with experience in working with the elderly (e.g., consultant pharmacists) or with specialized certification in geriatrics (e.g., certified geriatric pharmacist [CGP]) may be helpful in tailoring a medication regimen to target therapy to the problem, minimize side effects, and avoid drug interactions. When necessary, if there is serious and imminent risk of harm to self or others, antipsychotic medication intervention remains a useful and sometimes necessary option.6
Nonpharmacologic Interventions: Behavioral modification, adjustment of the environment (e.g., noise, temperature, disruption), group therapy, supportive psychotherapy, and recreational activities (e.g., music therapy, gardening), among other strategies, may be helpful in reducing or eliminating the need for pharmacologic intervention.
Consideration of the Nuances Between Individual Medications: Due to the broad categories of agents, this is required for rational prescribing and tailoring of psychotropic drug therapy to the individual geriatric patient.
Start Low, Go Slow, and Monitor Frequently: In the elderly, initial doses should be based on geriatric dosing guidelines, with gradual titration and close, frequent monitoring.
Ongoing Assessment for
Appropriate Adjustment of
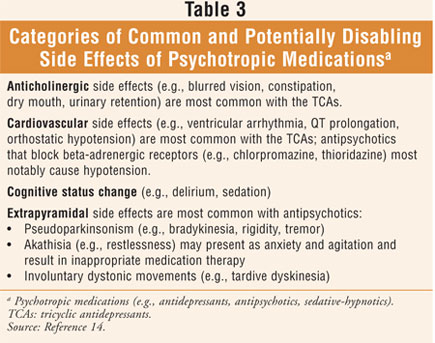
Psychotropic Drug Therapy Is Essential: Observation is required to detect a response of target symptoms to prescribed therapy. Additionally, the prescribing clinician should take into account reports from patients and caregivers and objective observations from trained professionals in an attempt to collect comprehensive data. Monitoring for common and potentially disabling side effects of psychotropic medications (TABLE 3) should be incorporated into the ongoing assessment process.
Any unexpected adverse events associated with antipsychotics should be reported to the FDA MedWatch program (www.fda.gov/medwatch/report/hcp.htm).3 Further, pharmacists should recommend the above-mentioned considerations, and weigh the risks versus the benefits of antipsychotic drug therapy, in the management of behavioral symptoms associated with dementia.
Conclusion
The FDA has determined new data provide evidence concluding the conventional antipsychotic agents share the increased risk of death in elderly patients with dementia-related psychosis that has been documented with the atypical antipsychotics. Currently, antipsychotic agents, whether conventional or atypical, are not indicated for the treatment of dementia-related psychosis. While antipsychotic agents may be a necessary option for certain circumstances, maximum caution is advised when these agents are prescribed in vulnerable individuals. For optimal care of seniors with dementia-related behavioral symptoms, a comprehensive, multifaceted approach is recommended while the quest for safer medications that are efficacious continues.
REFERENCES
1. ACNP White Paper: Update on Use of Antipsychotic Drugs in Elderly Persons With Dementia. Neuropsychopharmacology. 2007:1-14. www.acnp.org/asset.axd?id=40ed5fbf-b74e-444e-a926-49b4c5bc7069. Accessed October 8, 2008.
2. Jin H, Meyer JM, Jeste DV. Atypical antipsychotics and glucose dysregulation: a systematic review. Schizoph Res. 2004;71:195-212.
3. The FDA Information for Healthcare Professionals brochure. U.S. Food and Drug Administration. Center for Drug Evaluation and Research. www.fda.gov/cder/drug/InfoSheets/HCP/antipsychotics_conventional.htm.
Accessed October 8, 2008.
4. Gill SS, Bronskill SE, Normand SL. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007;146:775-786.
5. Schneeweiss S, Setoguchi S, Brookhart A. Risk of death associated with the use of conventional versus atypical antipsychotic drugs among elderly patients. CMAJ. 2007;176:627-632.
6. Pizzi DM. Black Box Warning Added to Older Antipsychotics. Pharmacy Practice News. August 2008:4-5.
7. Blass JP. Dementias Including Alzheimer's Disease. In: Hazzard WR, Blass JP, Halter JB, et al. Principles of Geriatric Medicine and Gerontology. 5th ed. New York, NY: McGraw-Hill, Inc; 2003:1391-1400.
8. Kaplan HI, Sadock BJ. Synopsis of Psychiatry. Baltimore, MD: Williams & Wilkins; 1998.
9. Evans DA, Funkenstein H, Albert MS, et al. Prevalence of Alzheimer's disease in a community population of older persons: higher than previously reported. J Am Med Assoc. 1989;262:2551-2556.
10. Losonczy KG, White LR, Brock DB. Prevalence and correlates of dementia: survey of the last days of life. Public Health Rep. 1998;113:273-280.
11. Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112-2117.
12. Wragg RE, Jeste DV. Neuroleptics and alternative treatments: management of behavioral symptoms and psychosis in Alzheimer's disease and related conditions. Psychiatr Clin North Am. 1988;11:195-214.
13. Lyketsos CG, Steinberg M, Tschanz JT, et al. Mental and behavioral disturbances in dementia: findings from the Cache County Study on memory in aging. Am J Psychiatry. 2000;157:708-714.
14. Kane RL, Ouslander JG, Abrass IB. Essentials of Clinical Geriatrics. 5th ed. New York, NY: McGraw-Hill, Inc; 2004:357-388.
15. Epocrates Rx Pro; version 8.10: updated October 9, 2008.
16. Semla TP, Beizer JL, Higbee MD. Geriatric Dosage Handbook. 12th ed. Hudson, OH: Lexi-Comp, Inc; 2007.
To comment on this article, contact rdavidson@jobson.com.





