US Pharm.
2008;33(3):48-58.
Scarlet fever is an infectious
disease caused by invasion of the upper respiratory tract by the Gram-positive
bacterium Streptococcus pyogenes.1 Ordinarily the resultant
illness is self-limiting, but more invasive infection that goes untreated can
be fatal. Scarlet fever was a serious, life-threatening disease for thousands
of children during the 19th century; it resulted in pandemics with substantial
mortality rates.2 One reason for this disproportionate loss of life
may have been misdiagnosis (as measles) or underdiagnosis.1,2
Scarlet fever, which typically affects children aged 2 to 10 years, is rare
due to exposure to S pyogenes by 10 years of age in most children.
3,4 The introduction of penicillin also contributed to the decreased
incidence of scarlet fever and its subsequent complications, such as rheumatic
fever; however, the decrease in incidence predates penicillin's introduction.
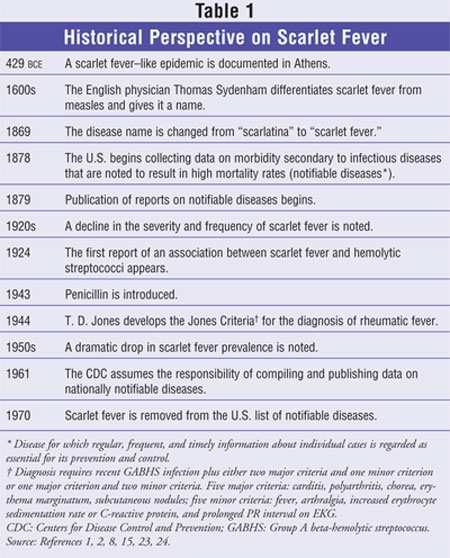
5 See TABLE 1 for a historical perspective on scarlet fever.
Since 1999, a total of 9,400
cases of scarlet fever have been reported in the United States by the Centers
for Disease Control and Prevention; 300 cases of streptococcal toxic shock
syndrome (STSS) and 600 cases of necrotizing fasciitis have been reported
during this period. These cases may be an under- or overestimation of
incidence because scarlet fever has not been a notifiable disease in the U.S.
since 1970.6 Approximately three million cases of strep throat
(acute pharyngitis and tonsillitis) and impetigo secondary to streptococcal
infection are reported yearly, however.6 The number of cases of
scarlet fever reported in 2004 in England and Wales, Scotland, and Northern
Ireland, respectively, wasÜ 2,200, 190, and 228.2
The causative organism, S
pyogenes, is classified as a Group A beta-hemolytic streptococcal (GABHS)
infection. It is the common cause of sore throat and fever associated with
strep throat and other skin infections (e.g., cellulitis, impetigo,
necrotizing faciitis, and erysipelas).7 Most cases of scarlet fever
are preceded by erythematous sore throat and fever; however, the disease can
result from other infectious illnesses, such as those associated with wounds
and burns.2
Transmission
GABHS is spread by
infected individuals during subclinical and acute illness via coughing,
sneezing, or aerosolizing respiratory droplets.2 With a brief
incubation time of two to four days, the bacterium propagates into the
bloodstream via the infected throat, wound, or burn.2,8 Without
antibiotic treatment, patients can be considered contagious for several weeks;
however, with treatment, communicability diminishes within 24 hours.9
Left untreated, the infectious period can last from 10 to 21 days.10
Signs and Symptoms
Clinical signs
associated with scarlet fever include manifestations of both the skin and the
soft tissue, such as a bright red (scarlet) rash, strawberry tongue (i.e.,
swollen red tongue with a white, fur-like coat and red, protruding papillae),
and lymphadenopathy.3,8 The onset of sore throat and fever
typically is sudden, with other symptoms, such as headache, chills, nausea,
vomiting, abdominal pain, and malaise, occurring shortly thereafter.
7,11,12 Upon examination, the tonsils are swollen, with yellow or
grayish-white exudate. The rash typically develops within one to two days of
disease onset; within two to three days the white coating on the tongue
resolves, leaving a raspberry tongue (i.e., bright red, swollen tongue with
large papillae).2,8
The Rash
The skin
manifestation of scarlet fever is theorized to be the result of erythrogenic
toxins produced by the bacteria that result in a delayed hypersensitivity
reaction.2,13 Most patients who develop this hypersensitivity
reaction have had prior exposure to GABHS.14 The nonpruritic,
painless rash is predominantly generalized along the skin folds of the trunk
in a linear formation (Pastia's lines), on the extremities, and in the
pharyngotonsillar area; 24 hours prior to this, its initial appearance is as
small red bumps on the axillae, groin, and neck.13,14 The cheeks
appear flushed, but the area around the mouth is pale.2 The rash
whitens when pressure is applied. The rash resembles sunburn and feels like
sandpaper; desquamation of the skin on the trunk, face, and fingertips occurs
during convalescence. Seven to 10 days after initial presentation, when the
fever abates, erythema decreases and desquamation of the trunk, face, and
fingertips begins; this may last for days to weeks as sheets of skin peel off
the face, torso, hands, and feet.8,11,15
Diagnosis
The confirmed
diagnosis of scarlet fever involves both symptoms (e.g., white blood cell
count >12,000/mm3, increased level of C-reactive protein) and
diagnostic tests. Several tests are available, including cultures of throat
secretions, rapid antigen-detection tests (RADTs), and streptococcal antibody
detection.8
Cultures of throat secretions
are necessary to differentiate viral from bacterial etiology of pharyngitis.
Both the tonsils and the posterior pharynx should be vigorously swabbed. If
throat swabs are taken correctly, the culture propagates GABHS in 90% to 95%
of patients with signs and symptoms.8 False-negative diagnosis
occurs in less than 10% of patients.9 Cultures that are negative
for GABHS for 24 hours should be incubated for a second day to ascertain that
the cultures really are negative.9
RADTs using throat swabs are
useful because results can be reported within hours of specimen collection.
8 The test detects nitrous acid extraction of group A carbohydrate
antigen from organisms in throat swabs.9 The specificity (i.e.,
ability of a test to correctly identify patients without the disease) of the
tests is high; however, the sensitivity (i.e., ability of a test to correctly
identify patients with the disease) of the tests varies.8
Therefore, if the RADT is negative, a confirmatory throat swab should be
ordered to make certain that the patient does not have group A streptococcal
(GAS) infection; positive tests do not need to be confirmed.9
Although RADTs are recommended by the American Academy of Pediatrics, the
Infectious Diseases Society of America, and the American Heart Association for
pediatric patients, recommendations for adult patients by the American College
of Physicians are controversial due to the test's lack of diagnostic precision.
8,16,17
Diagnosis of previous GABHS
infection can also be made by testing for streptococcal antibodies. Tests for
antistreptolysin O and anti-DNase B are used more frequently due to commercial
availability. Although these tests are not useful for acute infections,
previous exposure can be detected by determining the difference between
current antibody titers for a given individual and mean titers for a given
population. If the initial titer is 200 Units/mL, the majority of patients
experience a two-fold or greater increase in titers between acute and
convalescent phase values.8 This diagnostic test may be beneficial
for patients who present with recurrent infections.
The diagnosis of scarlet fever
can be determined by the severity of the patient's underlying symptoms. The
Health Protection Agency describes scarlet fever cases as confirmed, probable,
or possible.2 "Confirmed" cases are those with clinical symptoms
consistent with streptococcal sore throat (e.g., sore, red throat; headache;
swollen lymph nodes) and at least one characteristic sign of scarlet fever
(e.g., skin rash; strawberry tongue; flushing of the cheeks with a pale area
around the mouth and peeling of the skin) and a positive throat culture.2
"Probable" cases are those with clinical symptoms consistent with
streptococcal sore throat and at least one characteristic sign of scarlet
fever, with no throat swab performed or a swab performed that shows no
significant growth.2 Cases are defined as "possible" if clinical
symptoms are present with no characteristic signs of scarlet fever and no
throat swab is performed, or a swab is performed but fails to produce
significant growth.2 Milder forms of scarlet fever are also
referred to as scarlatina.2
Treatment
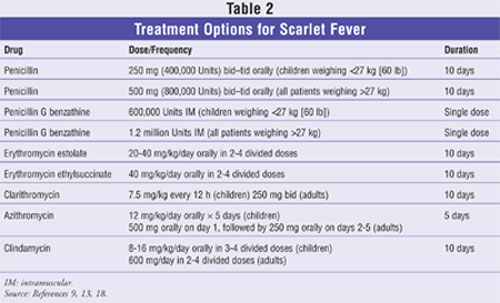
The drug of choice
for the treatment of scarlet fever is penicillin. The dose of orally
administered penicillin is 250 mg (400,000 Units) two to three times daily for
ten days for children weighing less than 27 kg (60 lb), and 500 mg (800,000
Units) two to three times daily for all other patients.2,3,9,11,18,19
A full course of 10 days is recommended to prevent the occurrence of acute
rheumatic fever.9 If nonadherence limits therapy, intramuscular
(IM) penicillin G benzathine is appropriate when given in a single dose of
600,000 Units for children who weigh less than 27 kg; all other patients
should receive 1.2 million Units. The pain from administration of the IM
formulation may be reduced by maintaining medications at room temperature
prior to injection.9 A combination of penicillin G benzathine
(900,000 Units) and penicillin G procaine (300,000 Units) is appropriate for
children; however, efficacy has not been demonstrated in adolescents and
adults.9
Patients who are allergic to
penicillin may take oral erythromycin unless bacterial resistance to
erythromycin is suspected. Erythromycin estolate (20-40 mg/kg/day orally in
two to four divided doses) or erythromycin ethylsuccinate (40 mg/kg orally per
day in two to four divided doses) should be administered over 10 days.
Clarithromycin or azithromycin administered for 10 or five days, respectively,
also may be considered.9 Oral cephalosporins may be considered for
patients who may be allergic to penicillin; however, the potential for
hypersensitivity to both penicillin and cephalosporin should be weighed in
patients with severe allergy to penicillin.
A patient who experiences
recurrence of symptoms shortly after completing a 10-day course of an
appropriate antibiotic can be re-treated with the same antibiotic or given an
alternative oral or IM antibiotic. Some alternatives are narrow-spectrum
cephalosporin, amoxicillin clavulanate, clindamycin, erythromycin, and other
macrolides; the order in which these antibiotics should be used has not been
clarified, however.9 Refer to TABLE 2 for treatment options
for scarlet fever.
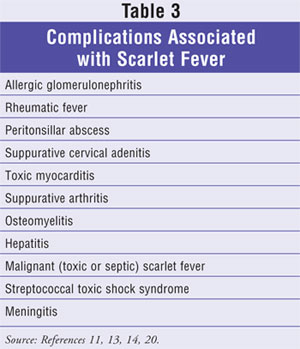
Complications
When scarlet fever is not treated
appropriately, several complications may occur, including allergic
glomerulonephritis, rheumatic fever, peritonsillar abscess, suppurative
cervical adenitis, toxic myocarditis, suppurative arthritis, osteomyelitis,
hepatitis, malignant (toxic or septic) scarlet fever, STSS, and meningitis.
11,13,14,20 Most complications occur early in the course of the disease;
however, late complications (e.g., allergic glomerulonephritis and rheumatic
fever) may occur two to three weeks after initial diagnosis.2 See
TABLE 3 for additional information on complications associated with
scarlet fever.
Severe forms of scarlet fever
and complications resulting from inappropriate treatment are extremely rare in
developed countries.10 These complications are not specific to
scarlet fever, as they may develop in patients who have other infections
caused by Streptococcus.11 Severe systemic reactions are thought to
be mediated by GABHS pyrogenic exotoxins.15 Fatalities from scarlet
fever are uncommon; only five deaths from streptococcal sore throat and
scarlatina were reported in the U.S. in 1983.1 The most severe
complications are discussed below.
Peritonsillar abscess is
caused by a combination of GAS and the formation of a polymicrobial abscess
that is predominated by anaerobic throat flora.8 The infection
typically responds to prompt drainage and treatment with penicillin. A patient
with an abscess experiences an abrupt increase in pain and dysphagia, neck
swelling, and fever after the initial symptoms of pharyngitis. Prompt
treatment is recommended to prevent fatal necrotizing fasciitis of the neck.
Several cases of hepatitis
have been reported as a complication of scarlet fever.15,21 In the
first case, a 9-year-old boy developed hepatitis that resolved after 20 days
of rehydration and bed rest.15 In another case report, two children
experienced hepatic complications of scarlet fever.21 The patient
in the first case was also receiving erythromycin, which is known to cause
hepatic dysfunction.18 However, hepatic complications have been
reported in patients diagnosed with scarlet fever who did not receive
erythromycin.
The incidence of STSS has
increased over the past decade. Patients with this severe complication, which
frequently results in death, present with hypotension, multiorgan failure, and
bacteremia. Necrotizing fasciitis and severe pain and tenderness may also
occur.14
During scarlet fever epidemics
in the 1950s, rheumatic fever developed in 3% of untreated patients.9
The incidence of rheumatic fever after endemic infection is believed to be
less than 1%. The risk of acute rheumatic fever can be eliminated by
appropriately treating scarlet fever infection; however, rare reports of
rheumatic fever when appropriate treatment was initiated have been described.
9
Three types of malignant
scarlet fever have been described, including anginose, hemorrhagic, and
atactic.22 These manifestations typically occurred before the
introduction of antibiotics, antipyrectics, and anticonvulsants. The anginose
form is characterized by membranous exudation of the throat with necrosis of
the soft tissues of the pharynx and soft palate. Exudation could extend into
the trachea, bronchi, eustachian tube, and middle ear. The necrosis was
reported to be so extensive in severe cases that necrosis of the carotid
artery occurred, with fatal hemorrhaging; death usually resulted in six to 14
days. Skin hemorrhaging, hematuria, and epistaxis occurred in patients with
the hemorrhagic form of scarlet fever. These symptoms typically occurred
within the first two to three days of the illness. Patients with atactic
scarlet fever presented with symptoms resembling acute intoxication. These
patients typically had fever as high as 108F, extreme restlessness, headache,
and delirium. Death usually occurred within 24 to 48 hours.20,22
Summary
Scarlet fever is a
rarely occurring infectious disease triggered by a hypersensitivity reaction
secondary to a GABHS pyrogenic toxin. Symptoms are usually mild. Patients with
scarlet fever initially present with sore throat, fever, and a scarlet rash.
The rash starts on the head and neck and then spreads to the trunk and
extremities. The rash is typically more marked in the skin folds of the trunk.
A distinctive feature of the rash is desquamation of the affected skin on the
torso, face, and extremities during recuperation.
Diagnosis of scarlet fever is
made based on patient symptoms and the presence of infection demonstrated by
diagnostic tests. After the diagnosis is confirmed, the drug of choice for
treating the infection is penicillin, although some other agents (i.e.,
erythromycin, cephalosporins, or clindamycin) can be used in patients who are
allergic to penicillin. Untreated scarlet fever can result in several
complications that can progress to death; therefore, prompt treatment is
necessary. Although scarlet fever is generally thought of as a disease of the
past, prompt and accurate diagnosis is necessary to prevent associated
complications.
REFERENCES
1. Quinn RW.
Comprehensive review of morbidity and mortality trends for rheumatic fever,
streptococcal disease, and scarlet fever: the decline of rheumatic fever.
Rev Infect Dis. 1989;11:928-953.
2. Marshall S. Scarlet
fever: the disease in the UK. Pharm J. 2006;277:115-116.
3. Aber C, Alvarez
Connelly E, Schachner LA. Fever and rash in a child: when to worry? Pediatr
Ann. 2007;36:30-38.
4. Davies RJ, deBono
JP. A young rash on old shoulders--scarlet fever in an adult male. Lancet
Infect Dis. 2002;2:750.
5. Pichichero ME,
McLinn SE, Gooch WM, et al. Ceftibuten vs. penicillin V in group A
beta-hemolytic streptococcal pharyngitis. Members of the Ceftibuten
Pharyngitis International Study Group. Pediatr Infect Dis J.
1995;14(suppl 7):S102-S107.
6. Centers for Disease
Control and Prevention. Group A streptococcal (GAS) disease. Available at:
www.cdc.gov/ncidod/dbmd/diseaseinfo/groupastreptococcal_g.htm. Accessed
December 17, 2007.
7. Merck Manual Online.
Streptococcal infections. Available at:
www.merck.com/mmhe/print/sec17/ch190/ch190s.html. Accessed December 27, 2007.
8. Stollerman GH.
Streptococcus pyogenes (group A streptococci). In: Gorbach SL, Bartlett JG,
Blacklow NR, eds. Infectious Diseases. 3rd ed. Philadelphia, PA:
Lippincott Williams & Wilkins; 2004:1596.
9. American Academy of
Pediatrics. Group A streptococcal infections. In: Pickering LK, Baker CJ, Long
SS, McMillan JA, eds. Red Book: 2006 Report of the Committee on Infectious
Diseases. 27th ed. Elk Grove Village, IL: American Academy of Pediatrics;
2006:610-619.
10. Hoek M, Dalling J,
Thompson S, et al. Scarlet fever outbreak in two nurseries in southwest
England. Euro Surveill. 2006;11:E060302.5.
11. Barnett BO, Frieden
IJ. Streptococcal skin diseases in children. Semin Dermatol.
1992;11:3-10.
12. Chiesa C, Pacifico
L, Nanni F, Orefici G. Recurrent attacks of scarlet fever. Arch Pediatr
Adolesc Med. 1994;148:656-660.
13. Hedrick J. Acute
bacterial skin infections in pediatric medicine: current issues in
presentation and treatment. Paediatr Drugs. 2003;5(suppl 1):35-46.
14. Weber DJ, Cohen MS,
Rutala WA. The acutely ill patient with fever and rash. In: Mandell GL,
Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases
. 6th ed. Philadelphia, PA: Elsevier; 2005;737-738.
15. Elishkewitz K,
Shapiro R, Amir J, Nussinovitch M. Hepatitis in scarlet fever. Isr Med
Assoc J. 2004;6:569-570.
16. Bisno AL, Gerber
MA, Gwaltney JM, et al. Practice guidelines for the diagnosis and management
of group A streptococcal pharyngitis. Infectious Diseases Society of America.
Clin Infect Dis. 2002;35:113-125.
17. Dajani A, Taubert
K, Ferrieri P, et al. Treatment of acute streptococcal pharyngitis and
prevention of rheumatic fever: a statement for health professionals.
Pediatrics. 1995;96:758-764.
18. Lexi-Drugs Online.
Available at: www.crlonline.com.ezproxy.samford.edu/crlonline. Accessed
December 19, 2007.
19. American Hospital
Formulary Service Online. Available at:
www.crlonline.com.ezproxy.samford.edu/crlonline. Accessed December 15, 2007.
20. Stevens DL.
Invasive group A streptococcus infections. Clin Infect Dis.
1992;14:2-11.
21. Girisch M,
Heininger U. Scarlet fever associated with hepatitis--a report of two cases.
Infection. 2000;28:251-253.
22. Stevens DL.
Invasive group A streptococcal infections: the past, present and future.
Pediatr Infect Dis J. 1994;13:561-566.
23. Dirckx JH, ed.
Stedman's Concise Medical Dictionary for the Health Professions. 4th ed.
Philadelphia, PA: Lippincott Williams & Wilkins; 2001.
24. McNabb SJN, Jajosky
RA, Hall-Baker PA, et al. Summary of notifiable diseases--United States, 2005.
MMWR. 2007;54:2-92.
To comment on this article, contact
editor@uspharmacist.com.





