US Pharm.
2008;33(7):23-25.
Along with the elderly
population's growth in numbers, there has been an increase in the number of
tuberculosis (TB) cases among seniors.1 While TB is preventable and
curable, approximately 1.5 million people died from it in 2006 according to
the World Health Organization (WHO).2 In addition, another 200,000
people died from HIV-associated TB.2 In the United States alone, a
total of 13,293 TB cases were reported in 2007.3 As a result of the
growth of TB-control programs nationwide, there has been a decline in the
overall number of reported TB cases in the U.S. within the last 10 years.4
In fact, the TB incidence rate in 2007 was the lowest recorded since national
reporting began in 1953.3 Despite these declines, however, the
elderly continue to account for a disproportionate share of the cases.4
If TB--an airborne infectious
disease--is diagnosed early and completely treated, patients with the disease
quickly become noninfectious and eventually cured.2 In elderly
patients, many clinical features of TB are subtle or absent, making diagnosis
difficult; the high number of cases diagnosed at autopsy among the
elderly suggests that TB frequently remains unrecognized.1,4
Compared with younger individuals, the mortality rate of TB in seniors is six
times higher.5 Pharmacists should take note that TB is a
preventable cause of death in seniors and should not be overlooked.5
The authors of one recent study suggested that an "increased awareness in
disease recognition and better medical and social support are
needed in addressing the problem of tuberculosis in older people."
1
Approximately three-quarters
of all TB cases in seniors occur in the respiratory tract.6
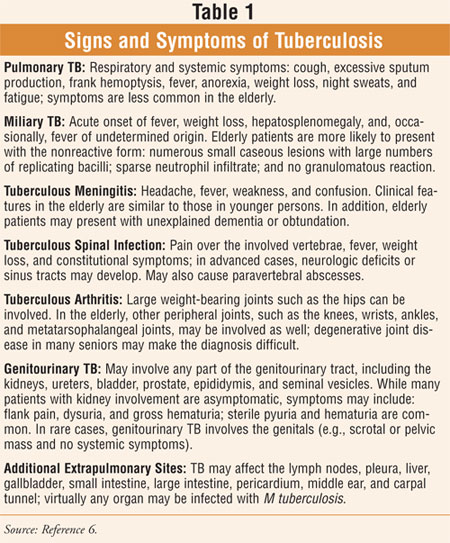
Extrapulmonary sites (TABLE 1) are common and include the bones and
joints (particularly the spine), and the genitourinary tract. A form of
disseminated TB, called miliary TB, is also relatively common in
seniors.6 According to WHO, major challenges associated with this
condition are multidrug-resistant TB (MDR-TB) and extensively drug-resistant
TB (XDR-TB), HIV-associated TB, and weak health systems.2 Further
challenges in the struggle against TB are faced by the WHO European Region: 1)
the high rate of multidrug–resistant TB (MDR-TB), mostly in the countries of
the former Soviet Union; 2) the rapid growth of the HIV epidemic in eastern
Europe and central Asia and, as a consequence, the sharp increase in
HIV-related TB; 3) the need to reform the health sector, to include closer
involvement of primary health care in TB control; 4) the still-limited
political and financial commitment to TB control; and 5) lack of advocacy,
communication, and social mobilization.7
TB Infection Versus TB
Disease
TB infection
is the term used to describe individuals who have contained the primary
infection and who remain asymptomatic with a positive tuberculin skin test.
6 Persons who have symptoms of infection are noted to have TB disease.
6 In 30% to 50% of cases, persistent TB infection is present without
disease.6 A loss of cellular immune reactivity (i.e., negative
tuberculin skin test) to Mycobacterium tuberculosis occurs in some
seniors who were previously infected with this organism, thereby
rendering them vulnerable to reinfection.6
In an attempt to adhere to the
national objective of elimination of this potentially curable disease, experts
recommend an aggressive approach to diagnosis, treatment, and prevention of TB
in the elderly.8 It has been reported that TB prophylaxis is
frequently withheld even when indicated, due to concern that elderly persons
are at greater risk for hepatic toxicity from TB treatment.4,8
Pharmacists can be assured, however, that the poor outcome of untreated TB in
this age-group warrants more aggressive treatment of the condition and that
through careful monitoring of seniors for adverse drug effects, successful
treatment may be achieved.4
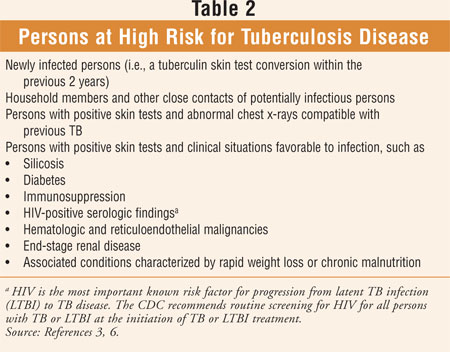
Those individuals at risk for
TB disease are outlined in TABLE 2. The most important known risk
factor for progression from latent TB infection (LTBI) to TB disease is HIV.
3 The CDC recommends routine screening for HIV for all persons with TB
or LTBI at the initiation of TB or LTBI treatment.3 The CDC
continues to work to increase national and international awareness of TB-HIV
coinfection and to improve the integration of TB-HIV health care services.
3
Signs and Symptoms
There is a major
concern surrounding TB in seniors regarding failure to recognize or diagnose
the disease.8 Classic features of TB, including cough, sputum
production, frank hemoptysis, fever, night sweats, and weight loss, may not be
exhibited in TB disease in the elderly (TABLE 1).5,6,8
Weight loss can occur; however, it is nonspecific.5 Clinical
features in the elderly may include anorexia, chronic fatigue, low-grade fever
(prolonged and unexplained), cognitive impairment, and changes in functional
ability (e.g., activities of daily living).8 Compared to younger
individuals, mental status changes are twice as common in seniors.5
Diagnosis
Tuberculin
Skin Test: Skin
testing with the Mantoux method is the standard screening procedure for TB
infection and reflects the delayed-type hypersensitivity response to M
tuberculosis antigen.6 Elderly patients with TB are far less
likely to present with positive skin tests.5
Chest X-ray:
Any lung segment can be
involved by primary TB; lung involvement for reactivated TB usually
includes the apical and posterior segments of the upper lobes and the superior
segments of the lower lobes.6 In the elderly, infiltrates may be
interstitial, lobar, patchy or cavitary, and bilateral.6
Laboratory Findings:
Clinical specimens
(e.g., sputum, urine) from suspected sites of TB are first examined by smear
to detect acid-fast bacilli and are subsequently cultured for M tuberculosis
.6 Serologic tests for antibody detection (i.e., against
mycobacterial antigens) have not been adequately refined for routine clinical
use.6
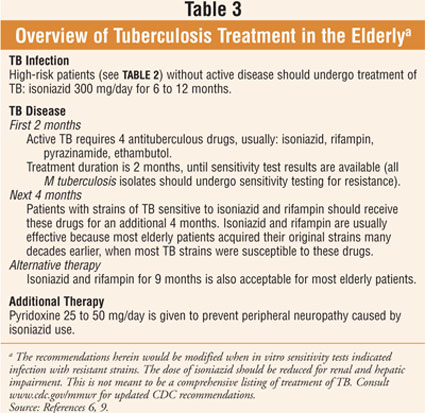
Treatment
An overview of the
treatment of TB in the elderly is provided in TABLE 3. Since
recommendations change due to resistant strains and newly developed
information, consulting MMWR (www.cdc.gov/mmwr) for current CDC
recommendations is advised.9 While the recommended treatment
duration is often the same for HIV-negative and HIV-positive patients, some
clinicians believe that the course of therapy should be extended for
immunocompromised patients.5 Treatment is extended by these
clinicians to nine months, rather than six months, to treat HIV-positive
patients with drug-susceptible TB.5 All TB patients should remain
under observation until adherence with their treatment regimen is established.
6 Although it is beyond the scope of this article to discuss the
pharmacologic management of TB in detail, the interested reader is referred to
Reference 6.
Monitoring
Monitoring with
laboratory parameters includes baseline liver enzyme, bilirubin, and serum
creatinine levels; a CBC; and a platelet count (or estimate).6
Monitoring of serum uric acid concentration is recommended when pyrazinamide
is part of the regimen.6 Patients should be monitored monthly for
symptoms of hepatitis (e.g., jaundice, fever, anorexia, dark urine, fatigue,
weakness, nausea, vomiting), a common adverse effect of isoniazid more
frequently seen in the elderly.6,9 During the first six months of
treatment, especially when hepatitis is most likely to occur, testing liver
function with aspartate transaminase is recommended.6 Isoniazid
should be discontinued if transaminase levels increase five or more times
higher than the upper limit of normal values.6 A U.S. Boxed Warning
for isoniazid states: "Severe and sometimes fatal hepatitis may occur or
develop even after many months of treatment."9 For patients
with active disease, sputum should be examined at least monthly until cultures
convert to negative; in approximately 90% of patients, cultures will convert
within three months of commencement of the recommended regimen.6,9
Evidence suggests that
institutionalized seniors are at a greater risk for reactivation of latent TB
and for the acquisition of new TB infection compared with their
community-dwelling counterparts.4 Patients in long-term care
facilities and acute-care institutions should be under surveillance, control,
and reporting for TB, according to CDC recommendations.6 Initial
skin testing and subsequent annual testing should be performed on all new
employees and new residents in long-term care facilities.6 The
initial comprehensive assessment of all elderly patients should include the
two-step purified protein derivative (PPD) screening.6 All persons
who test tuberculin positive on admission to a long-term care facility should
have a chest x-ray to ensure the absence of pulmonary infiltrates consistent
with TB.6 Furthermore, a chest x-ray should be performed on anyone
suspected of having TB.6
REFERENCES
1. Chand N, Bhushan
B, Singh D. Tuberculosis in the elderly (aged 50 years and above) and their
treatment outcome under DOTS. Chest.
http://meeting.chestjournal.org/cgi/ content/abstract/132/4/640b. Accessed
June 16, 2008.
2. A World Free of TB.
World Health Organization. www.who.int/tb/en/. Accessed June 16, 2008.
3. Trends in
Tuberculosis--United States, 2007. Centers for Disease Control. MMWR.
March 21, 2008. www.cdc.gov/mmwr/preview/mmwrhtml/mm5711a2.htm. Accessed June
16, 2008.
4. Zevallos M, Justman
JE. Tuberculosis in the elderly. Clin Geriatr Med. 2003 Feb;19:121-138.
5. Peloquin CA.
Tuberculosis. In: DiPiro JT, Talbert RL, Yee GC, et al, eds.
Pharmacotherapy: A Pathophysiologic Approach. 6th ed. New York, NY:
McGraw-Hill, Inc; 2005:2015-2034.
6. Tuberculosis. The
Merck Manual of Geriatrics. www.merck.com/mkgr/mmg/sec10/ch76/ch76b.jsp.
Accessed June 16, 2008.
7. Challenges for TB
control in the European Region. World Health Organization Regional Office for
Europe. www.euro.who.int/tuberculosis/issues/20030312_1. Accessed June 16,
2008.
8. Rajagopalan S,
Yoshikawa TT. Tuberculosis. In: Hazzard WR, Blass JP, Halter JB, et al, eds.
Principles of Geriatric Medicine and Gerontology. 5th ed. New York, NY:
McGraw-Hill, Inc; 2003:1099-1105.
9. Semla TP, Beizer JL,
Higbee MD. Geriatric Dosage Handbook. 12th ed. Hudson, OH: Lexi-Comp,
Inc; 2007.
To comment on this article,
contact
rdavidson@jobson.com.






