US Pharm. 2006;31(11)(Diabetes suppl):21-30.
Children
have historically been heavily impacted by diabetes. In the early decades of
the last century, before diabetes was recognized as being not one but many
distinct endocrine disorders, children were among the most frequently
diagnosed with those disease. Terms such as juvenile diabetes and
childhood-onset diabetes were used to describe what is now known as type 1
diabetes mellitus (DM). More recently, the number of children diagnosed with
type 2 DM, a disease formerly thought to be exclusive to adults, has exploded.
Diabetes is one of the most frequently diagnosed chronic diseases in children,
with more than 175,000 persons in the United States younger than 20 years
having some form of diabetes.1
Pharmacists have always been
integrally involved in the care of children with diabetes. For example, when
the Durham-Humphrey Amendment, enacted in 1951, defined the medications
requiring a physician's prescription, insulins were specifically excluded in
order to allow pharmacists to dispense these live-preserving treatments
without prior authorization. More recently, the Asheville Project diabetes
program, clinics that have pharmacotherapists on staff, and community
pharmacyñbased diabetes self-education classes highlight the continuing role
of pharmacists in caring for patients with diabetes. This review familiarizes
pharmacists with the many aspects of diabetes care relevant to children and
adolescents living with diseases in this family.
Type 1 DM in Children
Type 1 DM, or
insulin-dependent DM, is an autoimmune disease involving pancreatic
beta-cell destruction and resultant insulin-production deficiency. This
disease accounts for approximately 5% to 10% of all cases of diabetes.In the
U.S., its average age of onset is 14 years.2 The rate of beta-cell
destruction is variable but appears to be faster in young children than in
older patients. As a result, ketoacidosis is more likely to be the presenting
problem among children and adolescents at time of diagnosis than it is among
adults.3
Type 1 DM is treated with
multiple daily insulin injections (either three or four times a day) or with
basal/bolus insulin infusion devices (insulin pumps).3 Due to the
complexity of the interactions between glucose and insulin, meals, and
exercise, children with type 1 DM must test their blood glucose levels very
frequently. Even small changes in any of these factors can have a dramatic
impact on blood glucose, resulting in dangerously high or low levels. Children
should be counseled to check their blood glucose as directed by their
clinician and to pay special attention to readings taken when their daily
routine is changed. They should never miss meals or insulin doses, and they
should monitor blood glucose levels before and after exercise. Those with a
history of exercise-induced hypoglycemia or those participating in endurance
events should be counseled to check their glucose levels during exercise.
A less common variant of type
1 DM, idiopathic type 1 (or Flatbush) DM is diagnosed most often in
young African-American or Asian men. It is similar to autoimmune type 1 DM in
its clinical presentation but differs in that it is not associated with
detectable beta-cellñdestroying antibodies.2 The main clinical
difference between autoimmune type 1 DM and idiopathic type 1 DM is that those
with the idiopathic variant may have waxing and waning insulin production for
years after diagnosis, and as a result, frequent insulin dose adjustments are
needed.
Insulin Pump Therapy for
Type 1 DM:Insulin
delivered continuously through an insulin pump is an extremely successful
strategy for intensive diabetes management and is gaining widespread
acceptance in the U.S. Insulin pump therapy simulates the function of
beta-cells more closely than do multiple daily injections.3 An
insulin pump delivers a constant basal insulin infusion and has the ability to
deliver larger insulin boluses around mealtimes. The bolus rate and size can
be altered depending upon caloric intake, expected activities, and other
situations (e.g., illness, emotional trauma) that can impact insulin demands.
The many advantages of insulin pump therapy include better insulin
pharmacokinetics, individualization of insulin therapy, and greater freedom in
timing of meals. The use of insulin pump therapy requires great motivation for
frequent blood glucose monitoring, carbohydrate counting, and regular medical
visits. The use of insulin pump therapy among children with type 1 DM is
predicted to increase along with expanded insurance coverage.
Type 2 DM in Children
Once thought of as
adult-onset DM, type 2 DM is becoming more common in children and
adolescents; however, the significance of this increasing prevalence may be
underestimated, as the disease may be difficult to diagnose or confused with
other types of diabetes in children.4 The increase in type 2 DM in
children parallels the continued increase in overweight and obesity in the
U.S. In late 1970s, about 4% of children were overweight, compared to more
than 17% of children in 2004, with Mexican-American boys and girls and
African-American girls at greatest risk for overweight.5
Diagnosing type 2 DM is
difficult, since children are often asymptomatic or unaware of their symptoms.
Clinicians must rely on family history and physical parameters to consider
testing for type 2 DM and laboratory information for the diagnosis.4
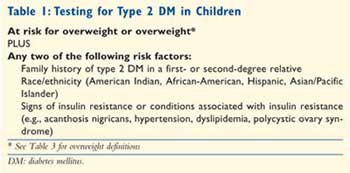
Criteria for testing children and adolescents for type 2 DM are described in
Table 1.
Correctly classifying a
child's diabetes type is critical to initiating appropriate treatment. The
predominant dysfunction in type 2 DM is insulin resistance.4
Therefore, medications that increase insulin sensitivity are most useful for
the treatment of this disease.
Lifestyle modification with
dietary intervention and physical activity are the primary management
strategies of type 2 DM in children. Depending on the severity of disease,
metformin (FDA approved for children 10 years and older) and/or insulin (at
bedtime, twice a day, or multidose regimens) may be the initial drug
treatment(s) in children with type 2 DM. For example, a child with
symptomatic, severe disease may begin insulin for most effective diabetes
control, followed by a titration to an oral medication. Conversely, a child
with asymptomatic but uncontrolled diabetes may use metformin initially. The
benefits of metformin over other oral agents for treatment of diabetes are a
decreased risk of hypoglycemia and possible weight and cholesterol reduction.
Clinical trials are evaluating thiazolidinediones in children; these agents
may eventually gain a role in the management of type 2 DM in children.6
Diabetes Complications and Concurrent
Diseases
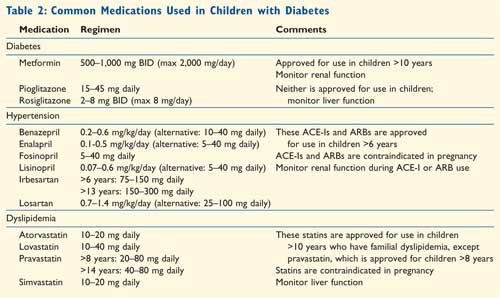
Many children and adolescents with diabetes may have microvascular complications and/or cardiovascular disease (CVD) risk factors. Control of weight, glucose, lipids, and blood pressure in children is necessary to prevent or delay development of complications and diseases.4 Common medications used to treat diabetes and associated diseases in children are listed in Table 2.
Diabetic retinopathy is damage
to blood vessels in the retina that eventually leads to vision loss and
blindness. Retinopathy may occur in both types of diabetes, although it is
found more frequently in children with type 1 DM than in those with type 2 DM.
7 Children with good glycemic control can be screened for retinopathy
every two years beginning at age 10 years and once the child has had type 1 DM
for three to five years. Adolescents with poor glycemic control, diabetes for
more than 10 years, or diagnosed retinopathy need more frequent screening.
8
Diabetic nephropathy is the
most common cause of chronic kidney disease in the U.S. Nephropathy may occur
more frequently in children with type 2 DM than in those with type 1 DM.7
Screening for microalbuminuria is recommended annually for both types of
diabetes beginning at the time of diagnosis of type 2 DM and beginning at age
10 years and once the child has had type 1 DM for five years.9
Screening should begin earlier (one year after diagnosis) for type 1 DM
diagnosed during adolescence, since puberty is an independent risk factor for
microalbuminuria.9 Confirmed elevated microalbumin levels may be
treated with angio!= tensin-converting enzyme inhibitors (ACE-Is), although
extreme caution is necessary when these agents are prescribed for sexually
active female adolescents due to the risk of fetal abnormalities.
Peripheral and autonomic
neuropathy caused by nerve damage occur at similar rates in children with type
1 or type 2 DM.7 Annual foot examinations should begin at puberty.
4
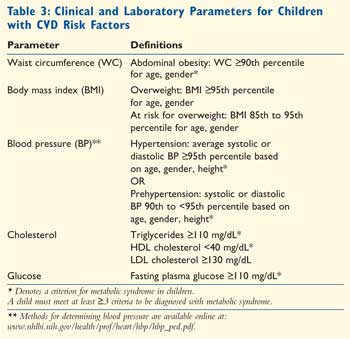
CVD risk factors are
prevalent in both types of diabetes, although a large waist circumference,
hypertension and high triglyceride and low HDL-cholesterol levels (National
Cholesterol Education Program Adult Treatment Panel III metabolic syndrome
criteria) occur at least three times more frequently in children and
adolescents with type 2 DM.10 Abdominal obesity and/or overweight
may directly impact the development of type 2 DM, hypertension, and
dyslipidemia.4 The clinical and laboratory parameters for CVD risk
factors are found in Table 3.
Dietary intervention and
physical activity, possibly along with pharmacologic therapy, are necessary to
prevent or delay the development of and to treat CVD risk factors.11
ACE-Is (or approved angiotensin II receptor blockers [ARBs]) are considered
first-line agents for treatment of hypertension in children with diabetes.
12 Pharmacologic treatment for prehypertension should be initiated if
goal blood pressure is not attained after three to six months of lifestyle
modifications.12 A fasting lipid panel should be obtained at
diagnosis once glucose control is established and followed every two years for
type 2 DM and every five years for type 1 DM if LDL† cholesterol remains at or
below 100 mg/dL.13
Management with statins is
indicated in children 10 years and older who are not at goal after six months
of lifestyle modification and have an LDL cholesterol level of at least 160
mg/dL, or 130 to 160 mg/dL with other CVD risk factors.13 Again,
fetal abnormalities may occur if statins are used in sexually active female
adolescents who become pregnant; thus, contraception is mandatory.
Emotional Impact of Diabetes
Regardless of age, children
diagnosed with diabetes often face tremendous emotional stress. Many of these
negative emotional effects are amplified in children and adolescents. They may
think themselves to be markedly different from their peers, a situation that
can lead to self-doubt and self-imposed isolation. It has been shown that
children with diabetes have a twofold increase in rates of depression, and
adolescents have a threefold increase, compared to those without diabetes.
14 Children with concurrent diabetes and depression have a tenfold
increase in suicide and suicidal ideation.14
Typically, a child diagnosed
with diabetes will report mild depression and anxiety immediately following
diagnosis, with resolution of these complaints six to 12 months later. These
depressive symptoms often return in one to two years. While boys usually lose
anxiety symptoms during the six years following diagnosis, girls often
demonstrate an increase in anxiety.3
Aside from the overall
negative impact of depression upon youth, depression negatively impacts
diabetes control. One recent study found that adolescents ages 13 to 18 with
psychiatric comorbidities had a significantly higher rate of diabetes-related
hospitalization than did those without.15 Interestingly, this
difference was not significant among younger children, which points toward the
greater impact of mood disorders among adolescents.
An important consideration
when treating a child with diabetes is appropriate self-management by age.
3 As children develop, it is important to allow them to accept more
responsibility for their own nutritional intake, monitoring, and treatment. A
child who is never allowed to care for himself or herself will not develop the
skills needed to cope with this lifelong disease. The pharmacist can aid in
the transition of care by always including the child and parent in educational
sessions.
Another troubling trend has
been that children entering adolescence while undergoing insulin therapy often
have body-image issues due to the adipose-forming effects of exogenous
insulin. As a result, some adolescents decrease or eliminate insulin therapy
in order to lose weight. The resultant acidosis can lead to rapid and profound
weight loss, further encouraging this dangerous activity, in the mind of the
patient. Pharmacists should pay close attention to adherence to insulin
therapy and should take notice of sudden or unexplained weight loss during the
adolescent and college years.
In addition to considering the
impact of diabetes on the mental health of the child, pharmacists should be
conscious of the emotional well-being of the parents or caregivers. For
instance, caring for an infant with diabetes dramatically increases the
already significant emotional toll on the parents.16 The complexity
of diabetes management plans and concerns of hypoglycemia may be overwhelming.
Pharmacists must take the time to question parents about their emotional and
mental health and refer for appropriate therapy as needed.
Pharmacist Involvement with Diabetes
By increasing their involvement in
caring for children with diabetes, pharmacists affirm their role as health
care leaders in the community. For instance, most regions of the country have
"diabetes camps," which provide a traditional camping experience to children
and adolescents with diabetes, in a medically supervised environment. These
camps enroll 15,000 to 20,000 children each year and can always use the
expertise of a pharmacist for dispensing medications and counseling the
children on their disease and its treatments.16 The Clinical
Practice Guidelines of the American Diabetes Association (ADA), published
every January in Diabetes Care, include guidelines for appropriate
management of these camps.17
These guidelines also include
recommendations for schools and daycare centers that enroll children with
diabetes.18 For instance, these institutions should design
individualized management plans that detail when a student may check his or
her glucose or administer medication and which activities the child may
participate in. Pharmacists can help ensure that school boards and
administrators adhere to these recommendations. The clinical practice
recommendations are available on the ADA Web site (www.diabetes.org).
Another valuable resource for
children with diabetes and their caregivers is the Children with Diabetes Web
site (www.childrenwithdiabetes.com). This site offers family support networks,
a question-and-answer forum, and recommendations for improving the quality of
life of a child with diabetes. Although this site does accept advertising, its
content is largely without commercial bias or influence, setting it apart from
many "informational" sites operated by pharmaceutical or monitoring device
manufacturers. One interesting component of this site is a set of formal
guidelines for babysitters of children with diabetes. Included are
recommendations (e.g., when and what to feed the child, when to give
medications, when to contact the parents) that should increase the comfort
level of both the parents and the babysitter.
Conclusion
Pharmacists have
ample opportunity to expand their role in the management of children and
adolescents with both type 1 and type 2 DM. A greater understanding of
diabetes and its complications along with associated CVD risk factors allows
pharmacists to become more proactive in screening, recommending and monitoring
pharmacologic therapy, and counseling children and adolescents with either
type 1 or type 2 DM. Pharmacists must also understand the emotional toll of
diabetes and be cognizant of the risk of depression in children and their
caregivers. Children with diabetes must be treated as much as possible like
children who do not have the disease in order to minimize the impact of
diabetes upon their quality of life. Beyond these standard components of
practice, pharmacists must also consider increasing their role in improving
community standards for the care of children living with diabetes.
References
1. American Diabetes Association. Standards of medical care in diabetes (Position Statement). Diabetes Care .2006;29:S4-S42.
2. American Diabetes Association. Diagnosis and classification of diabetes (Position Statement). Diabetes Care .2006;29:S43-S48.
3. American Diabetes Association. Care of children and adolescents with type 1 diabetes (Statement). Diabetes Care. 2005;28:186-212.
4. American Diabetes Association. Type 2 diabetes in children and adolescents (Consensus Statement). Diabetes Care.2000;23:381-389.
5. Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549-1555.
6. National Institute of Diabetes and Digestive and Kidney Diseases. Treatment options for type 2 diabetes in adolescents and youth (TODAY). Available from: www.todaystudy.org/medp1.cgi. Accessed March 30, 2005.
7. Eppens MC, Craig ME, Cusumano J, et al. Prevalence of diabetes complications in adolescents with type 2 compared to type 1 diabetes. Diabetes Care. 2006;29:1300-1306.
8. Maguire A, Chan A, Cusumano J, et al. The case for biennial retinopathy screening in children and adolescent. Diabetes Care. 2005;28:509-513.
9. Gross JL, DeAzevedo MJ, Silveiro AP. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005;28:164-176.
10. Rodriguez BL, Fujimoto WY, Mayer-Davis EJ. Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes. Diabetes Care. 2006;29:1891-1896.
11. Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
12. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555-575.
13. American Diabetes Association. Management of dyslipidemia in children and adolescents with diabetes (Consensus Statement). Diabetes Care. 2003;26:2194-2197.
14. Grey M, Whittemore R, Tamborlane W. Depression in type 1 diabetes in children; natural history and correlates. J Psychosom Res. 2002;53:907-911.
15. Garrison MM, Katon WJ, Richardson LP. The impact of psychiatric comorbidities on readmissions for diabetes in youth. Diabetes Care. 2005;28:2150-2154.
16. Banion CR, Miles MS, Carter MC. Problems of mothers in management of children with diabetes. Diabetes Care . 1983;6:548-551.
17. Diabetes care at diabetes camps. Diabetes Care. 2006;29:S56-S68.
18. Diabetes care in the school and
day care setting. Diabetes Care. 2006;29:S49-S55.
To comment on this article, contact
editor@uspharmacist.com.





