US
Pharm. 2006;4:28-32.
Dryness of the skin, known
as xerosis, or xeroderma, is a common condition in the elderly.
As people age, the outer layer of skin loses water, causing the surface to
become dry and rough.1 Incidence of xerosis increases with age, and
prevalence of the condition in the United States may increase, given the
demographic aging of the population.2 Xerosis may be a troubling
condition in elderly individuals because of its physical appearance and the
physical discomfort that may ensue. While the exact cause of xerosis is
unknown, the condition is related to altered lipid composition of the stratum
corneum, in addition to other changes in epidermal differentiation.1
It appears as though xerosis does not occur as a result of decreased water in
the skin, but rather is the result of abnormal keritinization and desquamation.
2
Signs and Symptoms
Although xerosis
is most prominent on the lower legs of patients who are middle-aged or older,
the condition also commonly presents on the trunk, forearms, and hands.
1,3 Xerosis may occasionally appear on the face, as well.2
Clinically, the skin appears tessellated (mosaic-like) with dull scales and
mild erythema.2 The skin also tends to itch and flake, which may be
distracting and distressful for some patients.4
Symptoms are usually
exacerbated in the winter because of low outdoor humidity due to cold
temperature and wind, and low indoor humidity due to central heating systems.
1 The stratum corneum loses excessive water under the condition of low
humidity, which dries the surface and makes the skin shiny and less pliable.
Once xerosis manifests, the condition tends to wax and wane with the
surrounding environmental conditions and persists indefinitely.2
Complications and
Differential Diagnosis
Dermatitis may result from the
drying effect of soaps, detergents, or other irritants (e.g., alcohol) that
are applied to the skin alone or are contained in skin care products.3,4
Dry skin may also fissure (crack). Irritating substances may enter the
fissures and excoriations, causing the skin to become red, itchy, swollen, or
painful.4 When this occurs, the condition is referred to as
eczema craquelé or asteatotic eczema.4 Pharmacists
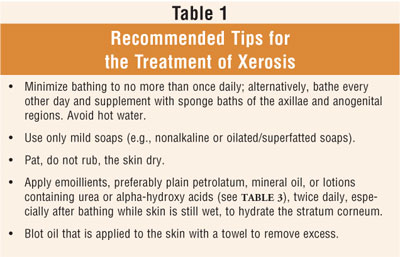
should encourage treatment interventions (table 1) to help patients avoid
complications and the possibility of further irritation, friction, and skin
breakdown, which may make the skin susceptible to infection.5
The differential diagnosis
of xerosis includes atopic eczema, autosomal dominant ichthyosis, nummular
eczema, and stasis dermatitis, as outlined in table 2. Inherited ichthyoses,
characterized by excessive accumulation of scales on the surface of the skin,
are classified according to clinical features such as age at onset (e.g.,
birth, infancy, or childhood), type of scale (e.g., fine, large and dark,
large and coarse, thick and warty), associated clinical findings (e.g.,
corneal opacities, ectropion, blisters) and genetic features (e.g., autosomal
dominant, X-linked, autosomal recessive). In these cases, it is recommended
that genetic counseling and treatment guidance be sought through consultation
with a dermatologist.3
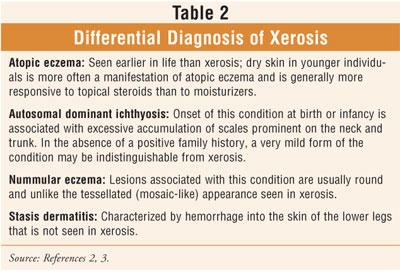
Very mild autosomal dominant
ichthyosis, in the absence of a positive family history, may in fact be
difficult to distinguish from xerosis.2 A diagnosis of acquired
ichthyosis may be an early manifestation of a systemic disease such as
hypothyroidism, lymphoma, leprosy, or AIDS. Fine scales may appear locally on
the trunk and legs or may be thick and widespread. Since the diagnosis of
xerosis is a clinical one, skin biopsy is usually not diagnostic. However, in
sarcoidosis, in which thick scales may be present on the legs, a biopsy
usually shows typical granulomas.
Importance of Maintaining
Skin Integrity in Seniors
Identifying and
addressing xerosis may be viewed as an integral part of maintaining skin
integrity. This is especially important in seniors, since aging skin
experiences anatomic changes resulting in altered physiologic behavior and
susceptibility to disease.6 Specifically, there is a decrease in
epidermal renewal, tissue repair, hair and nail growth, and the quantity of
eccrine, apocrine, and sebum secretion. As a person ages, a decrease in the
inflammatory response, absorption, and cutaneous clearance occurs due to a
decrease in cutaneous vascular supply. In fact, a prominent feature of aged
skin is the regression and disorganization of small vessels. Additionally,
thermal regulation, tactile sensitivity, and pain perception are all impaired
to some degree in the aging adult.6 Pharmacists can promote the
importance of skin integrity with recommendations regarding cleansing and
moisturization of the skin (table 1).
Prophylaxis and Treatment
In general, there
is a twofold approach to the treatment of xerosis: (1) minimizing irritation
and (2) moisturization.2 Patients should be instructed to limit
bathing, especially in soapy baths that strip oil from skin and leave it
chapped.2 While some experts recommend bathing once daily in warm
water and mild soap, others suggest bathing only every other day and
supplementing with sponge baths of the axillae and anogenital areas, since
these areas are rarely affected by xerosis.1,2 Patting the skin dry
instead of rubbing can also help. Detergents, rubbing alcohol, and skin care
products that contain alcohol and other drying agents should be avoided if
possible. Irritating materials (e.g., wool) should not be placed next to the
skin.1
In general, moisturization
through frequent and liberal application of emollients is recommended,
especially after bathing when water can be trapped in the skin with an
occlusive agent.2 Moisturizers have water-retaining and lubricating
properties and exhibit weak antipruritic, anti-inflammatory, antimitotic, and
vaso constrictive effects, which make them suitable treatments for
mildly eczematized xerotic skin.2 The generous and frequent
application of moisturizers that contain lanolin or white petrolatum
effectively traps and retains water in the skin.4 Scented
emollients are not recommended, to avoid skin irritation and contact
sensitization.1 Emollients have few side effects, usually confined
to contact dermatitis, folliculitis, and miliaria (cutaneous changes
associated with retention and discharge of sweat).2
Seniors should be informed
that while over-the-counter emollients vary greatly in quality and cost, there
is no strict relationship between the two.1 Checking labels for
ingredients known to be useful in the treatment of xerosis (table 3) should be
encouraged to avoid confusion from misleading claims and advertisements. Some
additives in expensive moisturizers, such as collagen and elastin, are used
for marketing, not
medical purposes, while other additives, such as vitamin E and fragrances, may
provoke an allergic dermatitis.2 An elegant, aesthetically
acceptable topical preparation may be advantageous for some patients who may
otherwise not adhere to a regimen that requires a thick, greasy ointment
(e.g., petrolatum) to be applied under their garments.
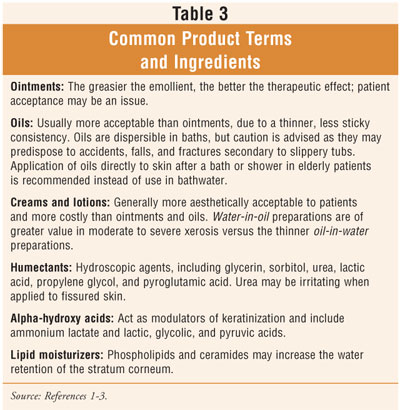
Creams and lotions that contain
urea or an alpha-hydroxy acid (table 3) are used to hydrate skin, remove
scales, and prevent symptoms.1 To increase indoor humidity during
the winter, a humidifier may be helpful. Topical cortico steroids may be
required if the skin becomes temporarily red, swollen, or painful.4
A low-potency topical steroid ointment (e.g., hydrocortisone 1% or 2.5%) is
recommended after bathing and at bedtime to treat inflamed, dry skin.1
Since ointments are more potent than creams that contain the same
corticosteroid in the same concentration, prolonged use of ointments is
discouraged due to systemic absorption.1 It is important to note
that topical steroids may actually provoke eczema craquelé in some
individuals.2
The pattern of xerosis has
been seen in some drug reactions.7 A drug may have the potential to
worsen xerosis by changing the chemical composition of the skin's outer layer.
4 This occurs most classically with those drugs used in the treatment of
hypercholesteremia, namely the HMG-CoA reductase inhibitors (statins), which
may cause severe xerosis.1,7
Conclusion
In aging skin,
anatomic changes result in altered physiologic behavior and susceptibility to
disease. Untreated, dry, itching, and scaling xerotic skin can fissure, making
a senior susceptible to red, chronically itchy, swollen, or painful skin.
Altered bathing habits, avoidance of
irritants, and adequate moisturization are the key treatment modalities for
xerosis. Topical steroids may be necessary if more conservative measures fail.
Pharmacists can assist by educating seniors about useful product categories.
Pharmacists may also appropriately recommend effective treatments that are
commensurate with a patient's aesthetic preferences and cost constraints.
REFERENCES
1. Beers MH,
Berkow R, eds. The Merck Manual of Geriatrics. 3rd ed. Whitehouse
Station, NJ: Merck & Co; 2000:1247-1248.
3. Beers MH, Berkow
R. The Merck Manual of Diagnosis and Therapy. 17th ed.
4. Beers MH, Jones
TV, Berkwits M, et al, eds. The Merck Manual of Health & Aging.
5.
6. Balin AK. Aging of
Human Skin. In: Hazzard WR, Andres R, Bierman EL. Principles of Geriatric
Medicine and Gerontology. 2nd ed.
7. Millikan LE. Drug
Eruptions. In: Newcomer VD, Young EM Jr. Geriatric Dermatology: Clinical
Diagnosis and Practical Therapy.
To comment on this article,
contact editor@uspharmacist.com.






